Hand & Wrist Injuries
Hand & wrist injuries are painful and inconvenient. It is important to quickly identify what your injury is and what your treatment options may be. Below you will find symptoms, treatment options, and other information about various hand & wrist injuries. Please contact us to request an orthopaedic evaluation.
Arthritis of the Hand & Arthritis of the Wrist
Arthritis is a common and sometimes debilitating condition caused by inflammation of the joints and resulting in pain and stiffness. Arthritis in the hand or wrist can make even simple daily activities more difficult.
Wrist
The wrist is made up of many small joints, and this can make it more prone to arthritis. Usually bones glide easily over each other when moved and are protected by a cartilage coating. Arthritis damages the cartilage and as the disease progresses, cartilage can be lost. The bones start rubbing on each other and can lead to permanent joint damage.
Hand
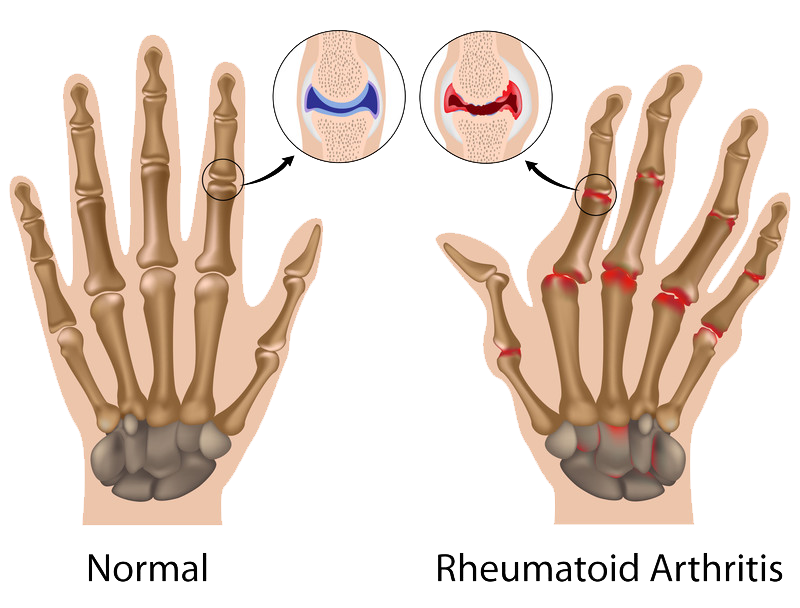
Like the wrist, the hand also has many small joints that work together with the wrist joints. The hand and wrist work together especially with fine motion such as tying a shoelace or knitting. When arthritis affects these joints it can have a major affect on daily activities. The most common forms of arthritis in the wrist and hand are osteoarthritis and rheumatoid arthritis.
Over time, untreated arthritis can cause deformities of the joints as well as chronic pain, inflammation, and the inability to perform certain activities.
Causes of Arthritis in the Wrist and Hand
Disease
The onset of arthritis is usually gradual if disease is the cause. The cartilage deteriorates slowly and the symptoms gradually increase. Osteoarthritis and rheumatoid arthritis are usually caused by disease.
Osteoarthritis is known to be caused by wear and tear over time. Rheumatoid arthritis can occur in many parts of the body and causes the joint lining (called synovium) to swell up and cause stiffness and pain in the joints. This form of arthritis often starts in the hands and feet, usually on the same side of the body.
Trauma
Dislocations or fractures that damage the surface of the joint are common injuries that can lead to the development of arthritis.
Symptoms
Pain
Dull or burning pain in the hand and wrist joints may indicate arthritis. The feeling may increase after heavy use of the joints, not immediately, but over several hours or the next day. Increased pain and stiffness in the morning is usual.
Swelling
When the affected joint is subject to greater stress than it can bear, it may swell in an attempt to prevent further joint use.
Deformity
Sometimes with severe arthritis the wrists or knuckles slip down, causing partial dislocation. This can give the wrists or thumb/fingers a deformed appearance.
Changes in Surrounding Joints
Sometimes advanced thumb base arthritis can cause the neighboring joints to become more mobile than normal.
Radiating Heat
The joint affected by arthritis may have a warm sensation and you may even feel heat by touching the skin. This is caused by the inflammation.
Grinding or Loose Feeling
Some patients report a sensation of grating or grinding in the affected joint (called crepitation). Damaged cartilage surfaces rubbing against one another causes this feeling. If the cause of the arthritis is damaged ligaments, the support structures of the joint may become loose. The joint area may look larger than normal due to swelling and changes in the bone and cartilage.
Formation of Cysts
Arthritis that affects the end joints of the fingers may cause small mucous cysts to develop. Evidence may also be seen as ridges or dents in the nail of the affected finger.
Surgical Options
When nonsurgical treatment fails to relive symptions, it’s time to consider surgery.
Surgery involves:
- Fusing the joints using a plate and screws at the base of the thumb. The surgeon will try to preserve or reconstruct the affected joint.
- Joint replacement or fusion is necessary if the damage is too severe. Joint fusions provide good pain relief, though they stop joint movement as the fused joint can no longer move. Joint replacement should provide pain relief and restore function.
Non-Surgical Options
Treatment options for arthritis of the hand and wrist depend on several factors, including:
- The progression of the arthritis
- The number of joints that are involved
- The overall health of the patient
- Whether it is the dominant or non-dominant hand that is affected
Medications
Medications cannot restore joint cartilage or reverse joint damage, but they can relieve symptoms. Anti-inflammatories are the usual medications used to help stop the body producing the chemicals that cause swelling and joint pain.
Injections
If anti-inflammatory medication does not offer relief, injections that contain a long-lasting anesthetic and a steroid can often provide temporary pain relief. Though the injections can be administered more than once, they are not suitable for ongoing use and may cause side effects.
Joint Support
By splinting the affected joint, stress on the joint may be eased and the symptoms may become less severe. The splint cannot be used for prolonged periods however, as muscle atrophy is a risk.
Carpal Tunnel Syndrome
Carpal tunnel syndrome is a common condition that causes pain, numbness, and tingling in the hand and arm. The condition occurs when one of the major nerves to the hand — the median nerve — is squeezed or compressed as it travels through the wrist.
In most patients, carpal tunnel syndrome gets worse over time, so early diagnosis and treatment are important. Early on, symptoms can often be relieved with simple measures like wearing a wrist splint or avoiding certain activities.
If pressure on the median nerve continues, however, it can lead to nerve damage and worsening symptoms. To prevent permanent damage, surgery to take pressure off the median nerve may be recommended for some patients.
Anatomy
The carpal tunnel is a narrow passageway in the wrist, about an inch wide. The floor and sides of the tunnel are formed by small wrist bones called carpal bones. The roof of the tunnel is a strong band of connective tissue called the transverse carpal ligament. Because these boundaries are very rigid, the carpal tunnel has little capacity to “stretch” or increase in size.

The median nerve is one of the main nerves in the hand. It originates as a group of nerve roots in the neck. These roots come together to form a single nerve in the arm. The median nerve goes down the arm and forearm, passes through the carpal tunnel at the wrist, and goes into the hand. The nerve provides feeling in the thumb and index, middle, and ring fingers. The nerve also controls the muscles around the base of the thumb.
The nine tendons that bend the fingers and thumb also travel through the carpal tunnel. These tendons are called flexor tendons.
Description
Carpal tunnel syndrome occurs when the tunnel becomes narrowed or when tissues surrounding the flexor tendons swell, putting pressure on the median nerve. These tissues are called the synovium. Normally, the synovium lubricates the tendons, making it easier to move your fingers.
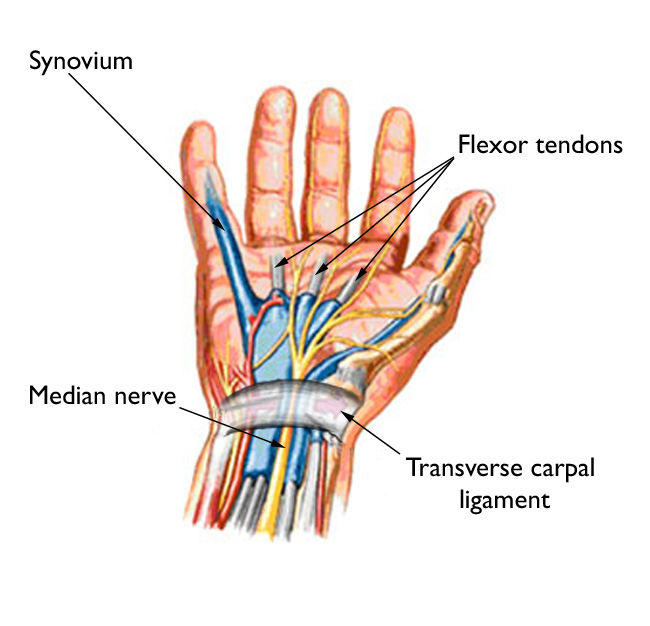
When the synovium swells, it takes up space in the carpal tunnel and, over time, crowds the nerve. This abnormal pressure on the nerve can result in pain, numbness, tingling, and weakness in the hand.
Cause
Most cases of carpal tunnel syndrome are caused by a combination of factors. Studies show that women and older people are more likely to develop the condition.
Other risk factors for carpal tunnel syndrome include:
- Heredity. This is likely an important factor. The carpal tunnel may be smaller in some people or there may be anatomic differences that change the amount of space for the nerve—and these traits can run in families.
- Repetitive hand use. Repeating the same hand and wrist motions or activities over a prolonged period of time may aggravate the tendons in the wrist, causing swelling that puts pressure on the nerve.
- Hand and wrist position. Doing activities that involve extreme flexion or extension of the hand and wrist for a prolonged period of time can increase pressure on the nerve.
- Pregnancy. Hormonal changes during pregnancy can cause swelling.
- Health conditions. Diabetes, rheumatoid arthritis, and thyroid gland imbalance are conditions that are associated with carpal tunnel syndrome.
Symptoms
Symptoms of carpal tunnel syndrome may include:
- Numbness, tingling, burning, and pain—primarily in the thumb and index, middle, and ring fingers
- Occasional shock-like sensations that radiate to the thumb and index, middle, and ring fingers
- Pain or tingling that may travel up the forearm toward the shoulder
- Weakness and clumsiness in the hand—this may make it difficult to perform fine movements such as buttoning your clothes
- Dropping things—due to weakness, numbness, or a loss of proprioception (awareness of where your hand is in space)
In most cases, the symptoms of carpal tunnel syndrome begin gradually—without a specific injury. Many patients find that their symptoms come and go at first. However, as the condition worsens, symptoms may occur more frequently or may persist for longer periods of time.
Night-time symptoms are very common. Because many people sleep with their wrists bent, symptoms may awaken you from sleep. During the day, symptoms often occur when holding something for a prolonged period of time with the wrist bent forward or backward, such as when using a phone, driving, or reading a book.
Many patients find that moving or shaking their hands helps relieve their symptoms.
Doctor Examination
During your evaluation, your doctor will talk to you about your general health and medical history and will ask about your symptoms.
He or she will carefully examine your hand and wrist and perform a number of physical tests. During these tests, your doctor will:
- Press down or tap along the median nerve at inside of your wrist to see if it causes any numbness or tingling in your fingers (Tinel sign)
- Bend and hold your wrists in a flexed position to test for numbness or tingling in your hands
- Test sensitivity in your fingertips and hands by lightly touching them with a special instrument when your eyes are closed.
- Check for weakness in the muscles around the base of your thumb
- Look for atrophy in the muscles around the base of your thumb. In severe cases, these muscles may become visibly smaller.
Tests
Electrophysiological tests. These tests will help your doctor measure how well your median nerve is working and help determine whether there is too much pressure on the nerve. The tests will also help your doctor determine whether you have another nerve condition, such as neuropathy, or other sites of nerve compression that might be contributing to your symptoms.
Electrophysiological tests may include:
Nerve conduction studies. These tests measure the signals travelling in the nerves of your hand and arm and can detect when a nerve is not conducting its signal effectively. Nerve conduction studies can help your doctor determine how severe your problem is and help to guide treatment.
Electromyogram (EMG). An EMG measures the electrical activity in muscles. EMG results can show whether you have any nerve or muscle damage.
Ultrasound. An ultrasound uses high-frequency sound waves to help create pictures of bone and tissue. Your doctor may recommend an ultrasound of your wrist to evaluate the median nerve for signs of compression.
X-rays. X-rays provide images of dense structures, such as bone. If you have limited wrist motion or wrist pain, your doctor may order x-rays to exclude other causes for your symptoms, such as arthritis, ligament injury, or a fracture.
Magnetic resonance imaging (MRI) scans. These studies provide better images of the body’s soft tissues. Your doctor may order an MRI to help determine other causes for your symptoms or to look for abnormal tissues that could be impacting the median nerve. An MRI can also help your doctor determine if there are problems with the nerve itself—such as scarring from an injury or tumor.
Treatment
Although it is a gradual process, for most people carpal tunnel syndrome will worsen over time without some form of treatment. For this reason, it is important to be evaluated and diagnosed by your doctor early on. In the early stages, it may be possible to slow or stop the progression of the disease.
Nonsurgical Treatment
If diagnosed and treated early, the symptoms of carpal tunnel syndrome can often be relieved without surgery. If your diagnosis is uncertain or if your symptoms are mild, your doctor will recommend nonsurgical treatment first.
Nonsurgical treatments may include:
Bracing or splinting. Wearing a brace or splint at night will keep you from bending your wrist while you sleep. Keeping your wrist in a straight or neutral position reduces pressure on the nerve in the carpal tunnel. It may also help to wear a splint during the day when doing activities that aggravate your symptoms.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Medications such as ibuprofen and naproxen can help relieve pain and inflammation.
Activity changes. Symptoms often occur when your hand and wrist are in the same position for too long—particularly when your wrist is flexed or extended.
If your job or recreational activities aggravate your symptoms, changing or modifying these activities can help slow or stop progression of the disease. In some cases, this may involve making changes to your work site or work station.
Nerve gliding exercises. Some patients may benefit from exercises that help the median nerve move more freely within the confines of the carpal tunnel. Specific exercises may be recommended by your doctor or therapist.
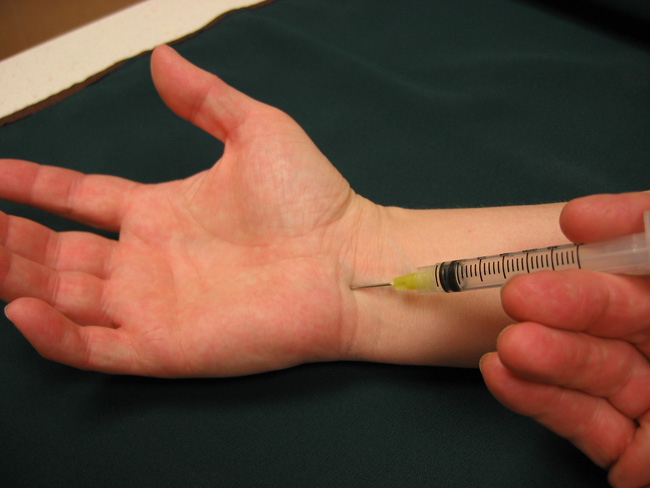
Steroid injections. Corticosteroid, or cortisone, is a powerful anti-inflammatory agent that can be injected into the carpal tunnel. Although these injections often relieve painful symptoms or help to calm a flare up of symptoms, their effect is sometimes only temporary. A cortisone injection may also be used by your doctor to help diagnose your carpal tunnel syndrome.
Surgical Treatment
If nonsurgical treatment does not relieve your symptoms after a period of time, your doctor may recommend surgery.
The decision whether to have surgery is based on the severity of your symptoms—how much pain and numbness you are having in your hand. In long-standing cases with constant numbness and wasting of your thumb muscles, surgery may be recommended to prevent irreversible damage.
Surgical Procedure
The surgical procedure performed for carpal tunnel syndrome is called a “carpal tunnel release.” There are two different surgical techniques for doing this, but the goal of both is to relieve pressure on your median nerve by cutting the ligament that forms the roof of the tunnel. This increases the size of the tunnel and decreases pressure on the median nerve.
In most cases, carpal tunnel surgery is done on an outpatient basis. The surgery can be done under general anesthesia, which puts you to sleep, or under local anesthesia, which numbs just your hand and arm. In some cases, you will also be given a light sedative through an intravenous (IV) line inserted into a vein in your arm.
Open carpal tunnel release. In open surgery, your doctor makes a small incision in the palm of your hand and views the inside of your hand and wrist through this incision. During the procedure, your doctor will divide the transverse carpal ligament (the roof of the carpal tunnel). This increases the size of the tunnel and decreases pressure on the median nerve.
After surgery, the ligament may gradually grow back together—but there will be more space in the carpal tunnel and pressure on the median nerve will be relieved.
Endoscopic carpal tunnel release. In endoscopic surgery, your doctor makes one or two smaller skin incisions—called portals—and uses a miniature camera—an endoscope—to see inside your hand and wrist. A special knife is used to divide the transverse carpal ligament, similar to the open carpal tunnel release procedure.
The outcomes of open surgery and endoscopic surgery are similar. There are benefits and potential risks associated with both techniques. Your doctor will talk with you about which surgical technique is best for you.
Recovery
Immediately following surgery, you will be encouraged to elevate your hand above your heart and move your fingers to reduce swelling and prevent stiffness.
You should expect some pain, swelling, and stiffness after your procedure. Minor soreness in your palm may last for several weeks to several months.
Grip and pinch strength usually return by about 2 to 3 months after surgery. If the condition of your median nerve was poor before surgery, however, grip and pinch strength may not improve for about 6 to 12 months.
You may have to wear a splint or wrist brace for several weeks. You will, however, be allowed to use your hand for light activities, taking care to avoid significant discomfort. Driving, self-care activities, and light lifting and gripping may be permitted soon after surgery.
Your doctor will talk with you about when you will be able to return to work and whether you will have any restrictions on your work activities.
Complications
Although complications are possible with any surgery, your doctor will take steps to minimize the risks. The most common complications of carpal tunnel release surgery include: bleeding, infection, and nerve aggravation or injury.
Trigger Finger
Trigger finger limits finger movement. When you try to straighten your finger, it will lock or catch before popping out straight.
Trigger finger is a condition that affects the tendons in your fingers or thumb.

Anatomy
Tendons are tissues that connect muscles to bone. When muscles contract, tendons pull on bones. This is what causes some parts of the body to move.
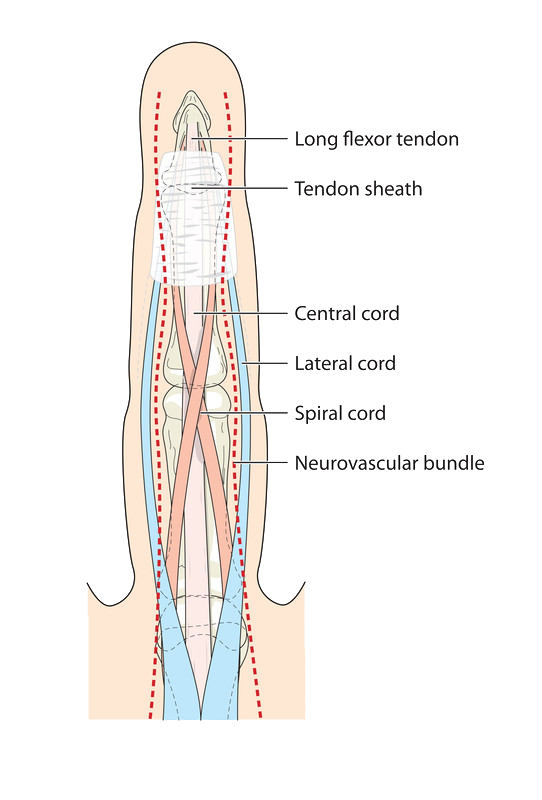
The muscles that move the fingers and thumb are located in the forearm, above the wrist. Long tendons — called the flexor tendons — extend from the muscles through the wrist and attach to the small bones of the fingers and thumb.
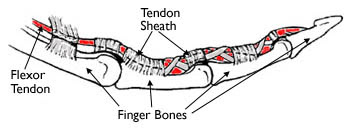
These flexor tendons control the movements of the fingers and thumb. When you bend or straighten your finger, the flexor tendon slides through a snug tunnel, called the tendon sheath, that keeps the tendon in place next to the bones.
Description
The flexor tendon can become irritated as it slides through the tendon sheath tunnel. As it becomes more and more irritated, the tendon may thicken and nodules may form, making its passage through the tunnel more difficult.
The tendon sheath may also thicken, causing the opening of the tunnel to become smaller.
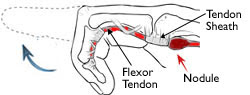
If you have trigger finger, the tendon becomes momentarily stuck at the mouth of the tendon sheath tunnel when you try to straighten your finger. You might feel a pop as the tendon slips through the tight area and your finger will suddenly shoot straight out.
Cause
The cause of trigger finger is usually unknown. There are factors that put people at greater risk for developing it.
- Trigger fingers are more common in women than men.
- They occur most frequently in people who are between the ages of 40 and 60 years of age.
- Trigger fingers are more common in people with certain medical problems, such as diabetes and rheumatoid arthritis.
- Trigger fingers may occur after activities that strain the hand.
Symptoms
Symptoms of trigger finger usually start without any injury, although they may follow a period of heavy hand use. Symptoms may include:
- A tender lump in your palm
- Swelling
- Catching or popping sensation in your finger or thumb joints
- Pain when bending or straightening your finger
Stiffness and catching tend to be worse after inactivity, such as when you wake in the morning. Your fingers will often loosen up as you move them.
Sometimes, when the tendon breaks free, it may feel like your finger joint is dislocating. In severe cases of trigger finger, the finger cannot be straightened, even with help. Sometimes, one or more fingers are affected.
Doctor Examination
Your doctor can diagnose the problem by talking with you and examining your hand. No other testing or x-rays are usually needed to diagnose trigger finger.
Nonsurgical Treatment
Rest.If symptoms are mild, resting the finger may be enough to resolve the problem. Your doctor may recommend a splint to keep your finger in a neutral, resting position.
Medications. Over-the-counter pain medications, such as non-steroidal anti-inflammatory medicines (NSAIDS) or acetaminophen can be used to relieve the pain.
Steroid Injections. Your doctor may choose to inject a corticosteroid — a powerful anti-inflammatory medication — into the tendon sheath. In some cases, this improves the problem only temporarily,and another injection is needed. If two injections fail to resolve the problem, surgery should be considered.
Injections are less likely to provide permanent relief if you have had the triggering for a long time, or if you have an associated medical problem, like diabetes.
Surgical Treatment
Trigger finger is not a dangerous condition. The decision to have surgery is a personal one, based on how severe your symptoms are and whether nonsurgical options have failed. In addition, if your finger is stuck in a bent position, your doctor may recommend surgery to prevent permanent stiffness.
Surgical Procedure
The goal of surgery is to widen the opening of the tunnel so that the tendon can slide through it more easily. This is usually done on an outpatient basis, meaning you will not need to stay overnight at the hospital.
Most people are given an injection of local anesthesia to numb the hand for the procedure.

The surgery is performed through a small incision in the palm or sometimes with the tip of a needle. The tendon sheath tunnel is cut. When it heals back together, the sheath is looser and the tendon has more room to move through it.
Complications
- Incomplete extension — due to persistent tightness of the tendon sheath beyond the part that was released
- Persistent triggering — due to incomplete release of the first part of the sheath
- Bowstringing — due to excessive release of the sheath
- Infection
Recovery
Most people are able to move their fingers immediately after surgery.
It is common to have some soreness in your palm. Frequently raising your hand above your heart can help reduce swelling and pain.
Recovery is usually complete within a few weeks, but it may take up to 6 months for all swelling and stiffness to go away.
If your finger was quite stiff before surgery, physical therapy and finger exercises may help loosen it up.
Symptoms
Symptoms may include:
- A tender lump that develops in the palm
- Swelling of the hand/fingers
- Popping or catching in finger or thumb joints
- Pain when straightening or bending the finger or thumb
- Stiffness in the morning that eases as the fingers are moved
Surgical Options
If a finger is stuck in a bent position a doctor may recommend surgery to prevent permanent stiffness.
Trigger finger surgery aims to widen the opening of the tunnel. This will help the tendon glide more easily. A small incision is made in the palm of the hand, allowing the doctor to cut the tendon sheath. As healing occurs the sheath becomes looser, allowing more room for the tendon’s movement.
Non-Surgical Options
- Rest If your condition isn’t too severe, you may find that resting the finger offers relief.
- A splint that helps keep your finger in a neutral position may also be recommended
Medications
- Anti-inflammatory medicines (NSAIDS) may help relieve the pain.
- Steroid injections- your doctor may recommend that corticosteroid be injected into the tendon sheath for temporary reduction of symptoms
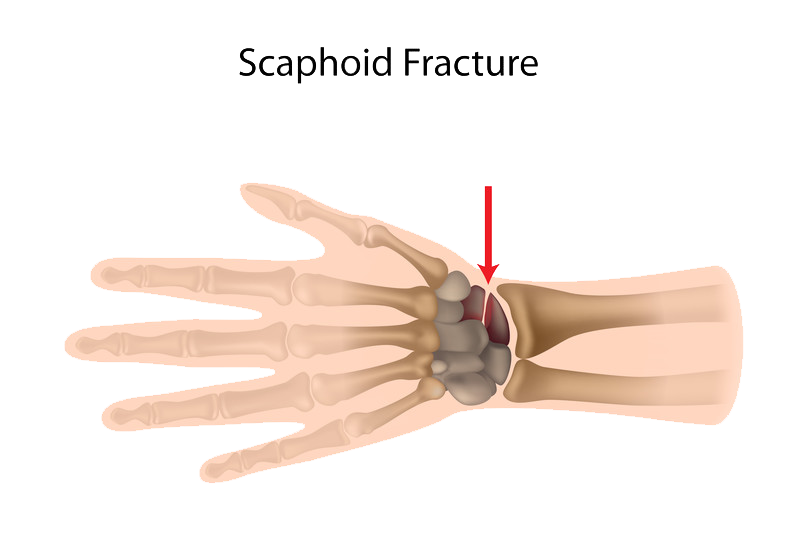
Hand Fractures & Wrist Fractures
A fracture is a broken bone. In the hand, a fracture commonly occurs in the small bones of the fingers or the longer bones called metacarpals. A fracture may occur from a fall, direct impact, crushing, or a twisting accident.
In the wrist, the break is usually in the distal radius, about one inch from the end of the bone. The bone may even tilt upwards. Other wrist fractures include:
Intra-Articular fracture
An intra-articular fracture is a fracture that extends into the wrist joint.
Extra-Articular fracture
An extra-articular fracture does not extend into the joint
Open fracture
An open fracture is when the bone actually breaks through the skin. These fractures require emergency attention due to immediate risk of infection.
Comminuted fracture
This is when a bone is broken into more than two pieces.
Symptoms
While a thorough investigation and X-ray is necessary to determine whether a hand fracture has occurred, the following are signs of fracture:
- Pain and tenderness in the hand
- Swelling
- Deformed or shorter appearance of the finger/thumb
- Inability to move the finger/thumb
- Fingers crossing over each other when trying to form a fist
- A further sign that is common in boxers is called a depressed knuckle. This is a fracture of the long bone below your little finger.
- In a wrist fracture, the hand may hang or bend unusually.
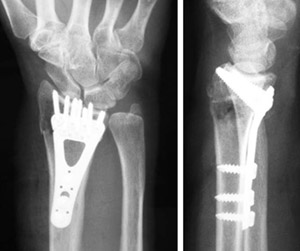
Surgical Options
Severe fractures may require surgery in order to re-align the bones and stabilize the hand and fingers. In some cases, the fractured bone may have gone through the skin, or the bone may be seriously shattered from a crushing injury. Dr. Sima is experienced in orthopaedic surgery procedures to repair all fractures and uses special plates, screws, and wires to hold the fractured bone in place while the injury heals.
When the bone has healed, the doctor will sometimes remove the implants. Care needs to be taken to ensure the joint doesn’t become too tight during the healing process. Special gentle exercises will be recommended to restore range of motion and regain strength.
Non-Surgical Options
Generally, bones can be manipulated by a qualified professional and realigned without needing an operation. The bones may be immobilized by use of a cast, brace, or splint until they can heal sufficiently. Reduction is the term given to the process in which the doctor moves the broken pieces back into the correct position. When a bone is straightened without having to operate, it is called a closed reduction.
Arthritis of the Thumb
Arthritis is a condition that irritates or destroys a joint. Although there are several types of arthritis, the one that most often affects the joint at the base of the thumb (the basal joint) is osteoarthritis (degenerative or “wear-and-tear” arthritis).
Description
Smooth cartilage covers the ends of the bones. It enables the bones to glide easily in the joint. Without it, bones rub against each other, causing friction and damage to the bones and the joint. Osteoarthritis occurs when the cartilage begins to wear away.
The joint at the base of the thumb, near the wrist and at the fleshy part of the thumb, enables the thumb to swivel, pivot, and pinch so that you can grip things in your hand.
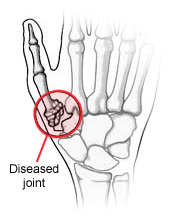
Arthritis of the base of the thumb is more common in women than in men, and usually occurs after 40 years of age. Prior fractures or other injuries to the joint may increase the likelihood of developing this condition.
Symptoms
- Pain with activities that involve gripping or pinching, such as turning a key, opening a door, or snapping your fingers
- Swelling and tenderness at the base of the thumb
- An aching discomfort after prolonged use
- Loss of strength in gripping or pinching activities
- An enlarged, “out-of-joint” appearance
- Development of a bony prominence or bump over the joint
- Limited motion
Doctor Examination
Your doctor will ask you about your symptoms, any prior injury, pain patterns, or activities that aggravate the condition.
One of the tests used during the examination involves holding the joint firmly while moving the thumb. If pain or a gritty feeling results, or if a grinding sound (crepitus) can be heard, the bones are rubbing directly against each other.
An x-ray may show deterioration of the joint as well as any bone spurs or calcium deposits that have developed.
Many people with arthritis at the base of the thumb also have symptoms of carpal tunnel syndrome, so your doctor may check for that, as well.
Nonsurgical Treatment
In its early stages, arthritis at the base of the thumb will respond to nonsurgical treatment.
- Ice the joint for 5 to 15 minutes several times a day.
- Take an anti-inflammatory medication, such as aspirin or ibuprofen, to help reduce inflammation and swelling.
- Wear a supportive splint to limit the movement of your thumb, and allow the joint to rest and heal. The splint may protect both the wrist and the thumb. It may be worn overnight or intermittently during the day.
Because arthritis is a progressive, degenerative disease, the condition may worsen over time. The next phase in treatment involves injecting a steroid solution injection directly into the joint. This will usually provide relief for several months. However, these injections cannot be repeated indefinitely.
Surgical Treatment
When nonsurgical treatment is no longer effective, surgery is an option. The operation can be performed on an outpatient basis, and several different procedures can be used.
One option involves fusing the bones of the joint together. This, however, will limit movement.
Another option is to remove part of the joint and reconstruct it using either a tendon graft or an artificial substance.
You and your physician will discuss the options and select the one that is best for you.
Rehabilitation
After surgery, you will have to wear a cast for 4 to 8 weeks, depending on which procedure is used. A rehabilitation program, often involving a physical therapist, helps you regain movement and strength in the hand. You may feel some discomfort during the initial stages of the rehabilitation program, but this will diminish over time. Full recovery from surgery takes several months. Most patients are able to resume normal activities.
Distal Radius Fracture
The radius is the larger of the two bones of the forearm. The end toward the wrist is called the distal end. A fracture of the distal radius occurs when the area of the radius near the wrist breaks.
Distal radius fractures are very common. In fact, the radius is the most commonly broken bone in the arm.
Description
A distal radius fracture almost always occurs about 1 inch from the end of the bone. The break can occur in many different ways, however.

One of the most common distal radius fractures is a Colles fracture, in which the broken fragment of the radius tilts upward. This fracture was first described in 1814 by an Irish surgeon and anatomist, Abraham Colles — hence the name “Colles” fracture.
Other ways the distal radius can break include:
- Intra-articular fracture. A fracture that extends into the wrist joint. (“Articular” means “joint.”)
- Extra-articular fracture. A fracture that does not extend into the joint is called an extra-articular fracture.
- Open fracture. When a fractured bone breaks the skin, it is called an open fracture. These types of fractures require immediate medical attention because of the risk for infection.
- Comminuted fracture. When a bone is broken into more than two pieces, it is called a comminuted fracture.
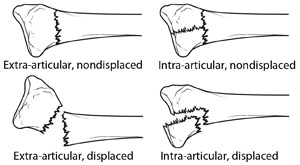
It is important to classify the type of fracture, because some fractures are more difficult to treat than others. Intra-articular fractures, open fractures, comminuted fractures, and displaced fractures (when the broken pieces of bone do not line up straight).are more difficult to treat, for example.
Sometimes, the other bone of the forearm (the ulna) is also broken. This is called a distal ulna fracture.
Cause
The most common cause of a distal radius fracture is a fall onto an outstretched arm.
Osteoporosis (a disorder in which bones become very fragile and more likely to break) can make a relatively minor fall result in a broken wrist. Many distal radius fractures in people older than 60 years of age are caused by a fall from a standing position.
A broken wrist can happen even in healthy bones, if the force of the trauma is severe enough. For example, a car accident or a fall off a bike may generate enough force to break a wrist.
Good bone health remains an important prevention option. Wrist guards may help to prevent some fractures, but they will not prevent them all.
Symptoms
A broken wrist usually causes immediate pain, tenderness, bruising, and swelling. In many cases, the wrist hangs in an odd or bent way (deformity).
Doctor Examination
If the injury is not very painful and the wrist is not deformed, it may be possible to wait until the next day to see a doctor. The wrist may be protected with a splint. An ice pack can be applied to the wrist and the wrist can be elevated until a doctor is able to examine it.
If the injury is very painful, if the wrist is deformed or numb, or the fingers are not pink, it is necessary to go to the emergency room.
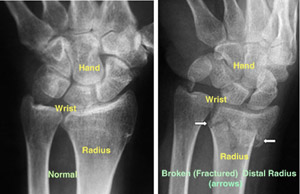
To confirm the diagnosis, the doctor will order x-rays of the wrist. X-rays are the most common and widely available diagnostic imaging technique. X-rays can show if the bone is broken and whether there is displacement (a gap between broken bones). They can also show how many pieces of broken bone there are.
Treatment
Treatment of broken bones follows one basic rule: the broken pieces must be put back into position and prevented from moving out of place until they are healed.
There are many treatment options for a distal radius fracture. The choice depends on many factors, such as the nature of the fracture, your age and activity level, and the surgeon’s personal preferences.
Nonsurgical Treatment
If the broken bone is in a good position, a plaster cast may be applied until the bone heals.
If the position (alignment) of your bone is out of place and likely to limit the future use of your arm, it may be necessary to re-align the broken bone fragments. “Reduction” is the technical term for this process in which the doctor moves the broken pieces into place. When a bone is straightened without having to open the skin (incision), it is called a closed reduction.
After the bone is properly aligned, a splint or cast may be placed on your arm. A splint is usually used for the first few days to allow for a small amount of normal swelling. A cast is usually added a few days to a week or so later, after the swelling goes down. The cast is changed 2 or 3 weeks later as the swelling goes down more, causing the cast to loosen.
Depending on the nature of the fracture, your doctor may closely monitor the healing by taking regular x-rays. If the fracture was reduced or thought to be unstable, x-rays may be taken at weekly intervals for 3 weeks and then at 6 weeks. X-rays may be taken less often if the fracture was not reduced and thought to be stable.
The cast is removed about 6 weeks after the fracture happened. At that point, physical therapy is often started to help improve the motion and function of the injured wrist.
Surgical Treatment
Sometimes, the position of the bone is so much out of place that it cannot be corrected or kept corrected in a cast. This has the potential of interfering with the future functioning of your arm. In this case, surgery may be required.
Surgery typically involves making an incision to directly access the broken bones to improve alignment (open reduction).
Depending on the fracture, there are a number of options for holding the bone in the correct position while it heals:
- Cast
- Metal pins (usually stainless steel or titanium)
- Plate and screws
- External fixator (a a stabilizing frame outside the body that holds the bones in the proper position so they can heal)
- Any combination of these techniques

Open fractures. Surgery is required as soon as possible (within 8 hours after injury) in all open fractures. The exposed soft tissue and bone must be thoroughly cleaned (debrided) and antibiotics may be given to prevent infection. Either external or internal fixation methods will be used to hold the bones in place. If the soft tissues around the fracture are badly damaged, your doctor may apply a temporary external fixator. Internal fixation with plates or screws may be utilized at a second procedure several days later.
Recovery
Because the kinds of distal radius fractures are so varied and the treatment options are so broad, recovery is different for each individual. Talk to your doctor for specific information about your recovery program and return to daily activities.
Pain Management
Most fractures hurt moderately for a few days to a couple of weeks. Many patients find that using ice, elevation (holding their arm up above their heart), and simple, non-prescription medications for pain relief are all that are needed to relieve pain.
Your doctor may recommend combining ibuprofen and acetaminophen to relieve pain and inflammation. The combination of both medications is much more effective than either one alone. If pain is severe, your doctor may suggest a prescription-strength medication, such as an opioid, for a few days.
Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Cast and Wound Care
In some cases, original casts will be replaced because swelling has gone down so much that the cast becomes loose. The last cast is usually removed after about 6 weeks.
During healing, casts and splints must be kept dry. A plastic bag over the arm while showering should help. If the cast does become wet, it will not dry very easily. A hair dryer on the cool setting may be helpful.
Most surgical incisions must be kept clean and dry for 5 days or until the sutures (stitches) are removed, whichever occurs later.
Potential Complications
After surgery or casting, it is important that you achieve full motion of your fingers as soon as possible. If you are not able to fully move your fingers within 24 hours due to pain and/or swelling, contact your doctor for evaluation.
Your doctor may loosen your cast or surgical dressing. In some cases, working with a physical or occupational therapist will be required to regain full motion.
Unrelenting pain may be a sign of Complex Regional Pain Syndrome (Reflex Sympathetic Dystrophy) which must be treated aggressively with medication or nerve blocks.
Rehabilitation and Return to Activity
Most people do return to all their former activities after a distal radius fracture. The nature of the injury, the kind of treatment received, and the body’s response to the treatment all have an impact, so the answer is different for each individual.
Almost all patients will have some stiffness in the wrist. This will generally lessen in the month or two after the cast is taken off or after surgery, and continue to improve for at least 2 years. If your doctor thinks it is needed, you will start physical therapy within a few days to weeks after surgery, or right after the last cast is taken off.
Most patients will be able to resume light activities, such as swimming or exercising the lower body in the gym, within 1 to 2 months after the cast is removed or within 1 to 2 months after surgery. Vigorous activities, such as skiing or football, may be resumed between 3 and 6 months after the injury.
Long-Term Outcomes
Recovery should be expected to take at least a year.
Some pain with vigorous activities may be expected for the first year. Some residual stiffness or ache is to be expected for 2 years or possibly permanently, especially for high-energy injuries (such as motorcycle crashes), in patients older than 50 years of age, or in patients who have some osteoarthritis. However, the stiffness is usually minor and may not affect the overall function of the arm.
Finally, osteoporosis is a factor in many wrist fractures. It has been suggested that people who have a wrist fracture should be tested for bone weakness, especially if they have other risk factors for osteoporosis. Ask your doctor about osteoporosis testing.
Dr. Sima has done bilateral carpal tunnel surgeries on me, and bilateral shoulder replacement. He is a outstanding physician, has a great bedside manner, and you feel you are in good hands. The results were excellent, and allowed me to continue my life with practically no pain, and resume playing piano again.
-Alan Satou