Knee Surgery
Surgery & Surgery Alternatives
Knee surgery may be the best option for your knee injury but there are surgery alternatives as well. We offer the latest in medical advancement to ensure that we find the best treatment for your injury or condition. Review knee surgery and surgery alternative options, success rates, recovery times and more below.
Surgical Knee Procedures
- Minimally Invasive Total Knee Replacement
- Autologous Chondrocyte Implantation (ACI)
- Anterior Cruciate Ligament Tears
- ACL Reconstruction
- Knee Ligament Reconstruction
- Knee Replacement (Partial or Total)
- Osteoarticular Transplant (OATS)
- Subchondroplasty (SCP)
- Microfracture
- Juvenile Cartilage Transplant
- Meniscal Tears
Minimally Invasive Total Knee Replacement
Minimally Invasive Total Knee Replacement
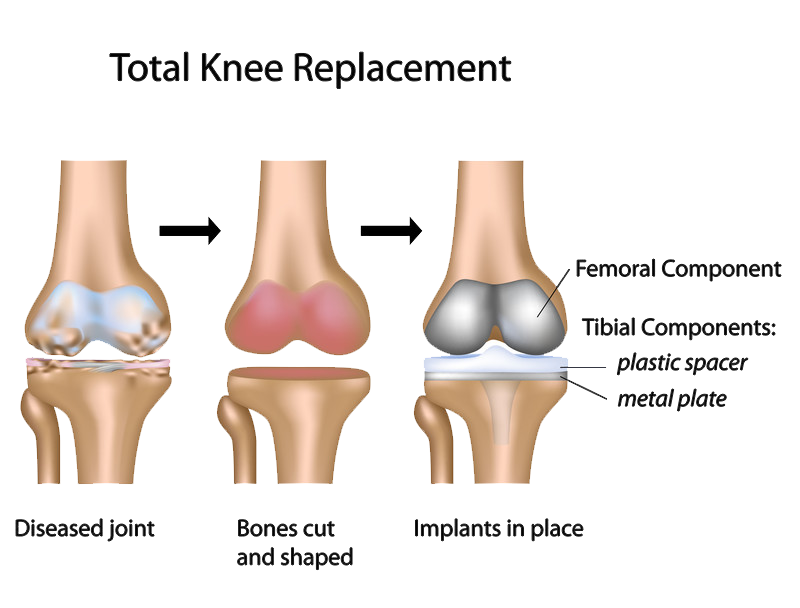
Total knee replacement (also called knee arthroplasty) is a common orthopaedic procedure that is used to replace the damaged or worn surfaces of the knee. Replacing these surfaces with an implant or “prosthesis” will relieve pain and increase mobility, allowing you to return to your normal, everyday activities.
The traditional approach to knee replacement uses a long vertical incision in the center of the knee to view and access the joint. Minimally invasive total knee replacement is a variation of this approach. The surgeon uses a shorter incision and a different, less-invasive technique to expose the joint—with the goal of reducing postoperative pain and speeding recovery.
Unlike traditional total knee replacement, the minimally invasive technique is not suitable for all patients. Your orthopaedic surgeon will discuss the different surgical options with you.
Description
During any knee replacement, the damaged cartilage and bone from the surface of the knee is removed, along with some soft tissues. The goal of knee replacement surgery is to provide the patient with a pain-free knee that allows for the return to daily activities and lasts for a long time.
Minimally invasive knee replacement differs from traditional knee replacement in that it uses an incision that is approximately half as long and fewer muscles are cut and detached.
Arthritis

The most common cause of chronic knee pain and disability is arthritis. Although there are many types of arthritis, most knee pain is caused by just three types: osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis.
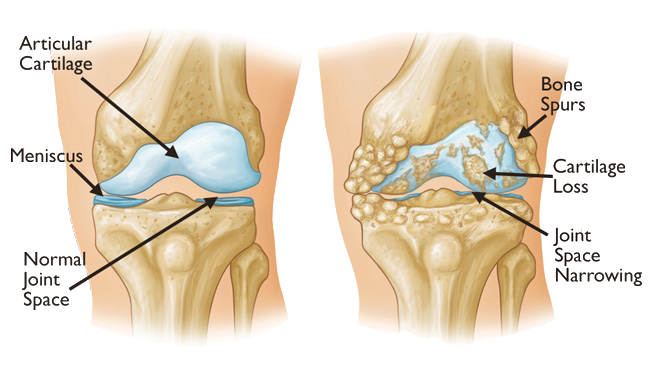
- Osteoarthritis. This is an age-related “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older, but may occur in younger people, too. The cartilage that cushions the bones of the knee softens and wears away. The bones then rub against one another, causing knee pain and stiffness.
- Rheumatoid arthritis. This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness. Rheumatoid arthritis is the most common form of a group of disorders termed “inflammatory arthritis.”
- Post-traumatic arthritis. This can follow a serious knee injury. Fractures of the bones surrounding the knee or tears of the knee ligaments may damage the articular cartilage over time, causing knee pain and limiting knee function.

- Severe knee pain or stiffness that limits your everyday activities, including walking, climbing stairs, and getting in and out of chairs. You may find it hard to walk more than a few blocks without significant pain and you may need to use a cane or walker
- Moderate or severe knee pain while resting, either day or night
- Chronic knee inflammation and swelling that does not improve with rest or medications
- Knee deformity — a bowing in or out of your knee
- Failure to substantially improve with other treatments such as anti-inflammatory medications, cortisone injections, lubricating injections, physical therapy, or other surgeries
Candidates for Surgery
There are no absolute age or weight restrictions for total knee replacement surgery. Recommendations for surgery are based on a patient’s pain and disability, not age. Most patients who undergo total knee replacement are age 50 to 80, but orthopaedic surgeons evaluate patients individually. Total knee replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
Minimally Invasive Knee Replacement
In minimally invasive knee replacement, the surgical procedure is similar, but there is less cutting of the tissue surrounding the knee. The artificial implants used are the same as those used for traditional knee replacement. However, specially designed surgical instruments are used to prepare the femur and tibia and to place the implants properly.
Minimally invasive knee replacement is performed through a shorter incision—4 to 6 inches versus 8 to 10 inches for traditional knee replacement. A smaller incision allows for less tissue disturbance.
In addition to a shorter incision, the technique used to open the knee is less invasive. In general, techniques used in minimally invasive knee replacement are “quadriceps sparing,” meaning they avoid trauma to the quadriceps tendon and muscles in the front of the thigh. Other minimally invasive techniques called “midvastus” and “subvastus” make small incisions in the muscle but are also less invasive than traditional knee replacement. Because the techniques used to expose the joint involve less disruption to the muscle, it may lead to less postoperative pain and reduced recovery time.
The hospital stay after minimally invasive surgery is similar in length to the stay after traditional knee replacement surgery–ranging from 1 to 4 days. Physical rehabilitation is a critical component of recovery. Your surgeon or a physical therapist will provide you with specific exercises to help increase your range of motion and restore your strength.
Candidates for Minimally Invasive Total Knee Replacement
Minimally invasive total knee replacement is not suitable for all patients. Your doctor will conduct a thorough evaluation and consider several factors before determining if the procedure is an option for you.
In general, candidates for minimal incision procedures are thinner, younger, healthier and more motivated to participate in the rehabilitation process, compared with patients who undergo the traditional surgery.
Minimally invasive surgeries may be less suitable for patients who are overweight or who have already undergone other knee surgeries.
In addition, patients who have a significant deformity of the knee, those who are very muscular, and those with health problems that may slow wound healing may be at a higher risk for problems from minimally invasive total knee replacement.
Iovera° Treatment
We also offer Iovera treatment. If your knee pain is chronic, due to osteoarthritis, it can be alleviated by cryoanalgesia with the iovera° treatment. The iovera° system has also been shown to help in reducing opioid consumption in patients after surgery. Postsurgical pain is considered to be acute pain.
The iovera° treatment is a focused therapy; therefore, there are no side effects to the entire body. Nothing is injected into the treatment area by the iovera° system. Therefore, very few, if any, localized side effects due to the iovera° treatment have been observed and side effects are mild.
Conclusion
Minimally invasive knee replacement is an evolving area and more research is needed on the long-term function and durability of the implants.
The benefits of minimally invasive knee replacement have been reported to include less damage to soft tissues, leading to a quicker, less painful recovery and more rapid return to normal activities. Current evidence suggests that the long-term benefits of minimally invasive surgery do not differ from those of knee replacement performed with the traditional approach.
Like all surgery, minimally invasive surgery has a risk of complications. These complications include nerve and artery injuries, wound healing problems, infection, and errors in positioning the prosthetic knee implants.
Like traditional knee replacement surgery, minimally invasive surgery should be performed by a well-trained, highly experienced orthopaedic surgeon. Your orthopaedic surgeon can talk to you about his or her experience with minimally invasive knee replacement surgery, and the possible risks and benefits of the techniques for your individual treatment.
Autologous Chondrocyte Implantation (ACI)
Autologous chondrocyte implantation (ACI) is state-of-the-art procedure that has recently been developed to treat cartilage, knee, and joint problems within the body.
How does ACI Work?
ACI takes place over a series of procedures
Stage One
- First, through arthroscopic surgery, your surgeon will take a very small section of articular cartilage from your knee in a procedure that takes less than 30 minutes.
- The articular cartilage sample is taken to a laboratory and treated in order to separate the chondrocytes (the cells that produce cartilage in our bodies).
- After 3 – 5 weeks (once the cells from the articular cartilage sample have multiplied), they are returned to the surgeon for the second procedure.
Stage Two
- The surgeon makes the damaged area of the knee smooth and covers it with a small patch of membrane.
- The chondrocytes that were cultured in the laboratory are then injected under the membrane.
- Over time, the cells will grow and settle into the joint, replacing the damaged area with new, healthier cartilage
The overall success rate of ACI is approximately 85% and allows patients to return to pain-free activities.
Anterior Cruciate Ligament Tears
The information that follows includes the details of anterior cruciate ligament (ACL) anatomy and the pathophysiology of an ACL tear, treatment options for ACL injuries along with a description of ACL surgical techniques and rehabilitation, potential complications, and outcomes. The information is intended to assist the patient in making the best-informed decision possible regarding the management of ACL injury.
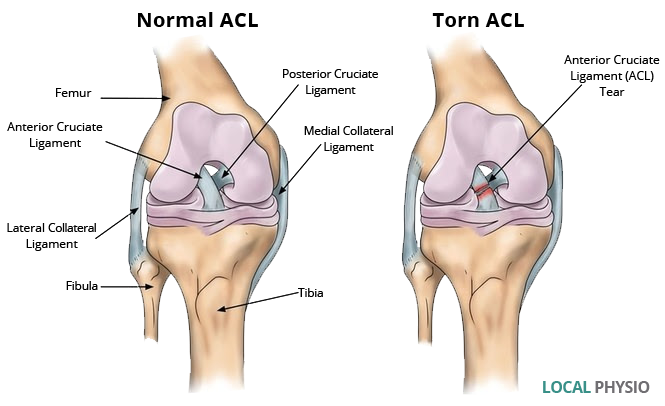
Anatomy
The bone structure of the knee joint is formed by the femur, the tibia, and the patella. The ACL is one of the four main ligaments within the knee that connect the femur to the tibia.
The knee is essentially a hinged joint that is held together by the medial collateral (MCL), lateral collateral (LCL), anterior cruciate (ACL) and posterior cruciate (PCL) ligaments. The ACL runs diagonally in the middle of the knee, preventing the tibia from sliding out in front of the femur, as well as providing rotational stability to the knee.
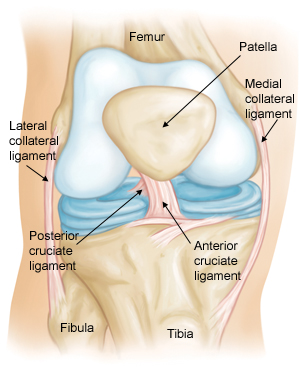
The weight-bearing surface of the knee is covered by a layer of articular cartilage. On either side of the joint, between the cartilage surfaces of the femur and tibia, are the medial meniscus and lateral meniscus. The menisci act as shock absorbers and work with the cartilage to reduce the stresses between the tibia and the femur.
Description
The anterior cruciate ligament (ACL) is one of the most commonly injured ligaments of the knee. The incidence of ACL injuries is currently estimated at approximately 200,000 annually, with 100,000 ACL reconstructions performed each year.1, 2 In general, the incidence of ACL injury is higher in people who participate in high-risk sports, such as basketball, football, skiing, and soccer.3, 4, 5

Approximately 50 percent of ACL injuries occur in combination with damage to the meniscus, articular cartilage, or other ligaments. Additionally, patients may have bruises of the bone beneath the cartilage surface. These may be seen on a magnetic resonance imaging (MRI) scan and may indicate injury to the overlying articular cartilage.20, 21
Cause
It is estimated that 70 percent of ACL injuries occur through non-contact mechanisms while 30 percent result from direct contact with another player or object.4
The mechanism of injury is often associated with deceleration coupled with cutting, pivoting or sidestepping maneuvers, awkward landings or “out of control” play.4, 7, 8, 9
Several studies have shown that female athletes have a higher incidence of ACL injury than male athletes in certain sports.3, 10 It has been proposed that this is due to differences in physical conditioning, muscular strength, and neuromuscular control. Other hypothesized causes of this gender-related difference in ACL injury rates include pelvis and lower extremity (leg) alignment, increased ligamentous laxity, and the effects of estrogen on ligament properties.4, 11, 12, 13, 14, 15, 16, 17, 18, 19
Immediately after the injury, patients usually experience pain and swelling and the knee feels unstable. Within a few hours after a new ACL injury, patients often have a large amount of knee swelling, a loss of full range of motion, pain or tenderness along the joint line and discomfort while walking.
Doctor Examination
When a patient with an ACL injury is initially seen for evaluation in the clinic, the doctor may order X-rays to look for any possible fractures. He or she may also order a magnetic resonance imaging (MRI) scan to evaluate the ACL and to check for evidence of injury to other knee ligaments, meniscus cartilage, or articular cartilage.
In addition to performing special tests for identifying meniscus tears and injury to other ligaments of the knee, the physician will often perform the Lachman’s test to see if the ACL is intact.
If the ACL is torn, the examiner will feel increased forward (upward or anterior) movement of the tibia in relation to the femur (especially when compared to the normal leg) and a soft, mushy endpoint (because the ACL is torn) when this movement ends.
Another test for ACL injury is the pivot shift test. In this test, , the tibia will start forward when the knee is fully straight and then will shift back into the correct position in relation to the femur when the knee is bent past 30 degrees.22
If the ACL is torn, the examiner will feel increased forward (upward or anterior) movement of the tibia in relation to the femur (especially when compared to the normal leg) and a soft, mushy endpoint (because the ACL is torn) when this movement ends.
Another test for ACL injury is the pivot shift test. In this test, , the tibia will start forward when the knee is fully straight and then will shift back into the correct position in relation to the femur when the knee is bent past 30 degrees.22
Natural History
The natural history of an ACL injury without surgical intervention varies from patient to patient and depends on the patient’s activity level, degree of injury and instability symptoms.
The prognosis for a partially torn ACL is often favorable, with the recovery and rehabilitation period usually at least three months. However, some patients with partial ACL tears may still have instability symptoms. Close clinical follow-up and a complete course of physical therapy helps identify those patients with unstable knees due to partial ACL tears.
Complete ACL ruptures have a much less favorable outcome. After a complete ACL tear, some patients are unable to participate in cutting or pivoting-type sports, while others have instability during even normal activities, such as walking. There are some rare individuals who can participate in sports without any symptoms of instability. This variability is related to the severity of the original knee injury, as well as the physical demands of the patient.
About half of ACL injuries occur in combination with damage to the meniscus, articular cartilage or other ligaments. Secondary damage may occur in patients who have repeated episodes of instability due to ACL injury. With chronic instability, up to 90 percent of patients will have meniscus damage when reassessed 10 or more years after the initial injury. Similarly, the prevalence of articular cartilage lesions increases up to 70 percent in patients who have a 10-year-old ACL deficiency.23, 24, 25, 26, 27, 28, 29, 30, 31, 32
Nonsurgical Treatment
In nonsurgical treatment, progressive physical therapy and rehabilitation can restore the knee to a condition close to its pre-injury state and educate the patient on how to prevent instability.37, 38 This may be supplemented with the use of a hinged knee brace. However, many people who choose not to have surgery may experience secondary injury to the knee due to repetitive instability episodes.
Surgical treatment is usually advised in dealing with combined injuries (ACL tears in combination with other injuries in the knee). However, deciding against surgery is reasonable for select patients. Nonsurgical management of isolated ACL tears is likely to be successful or may be indicated in patients:
- With partial tears and no instability symptoms39
- With complete tears and no symptoms of knee instability during low-demand sports who are willing to give up high-demand sports
- Who do light manual work or live sedentary lifestyles
- Whose growth plates are still open (children)
Surgical Treatment
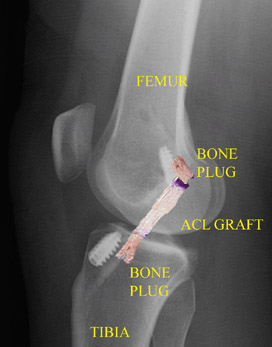
ACL tears are not usually repaired using suture to sew it back together, because repaired ACLs have generally been shown to fail over time.31, 33, 34, 35, 36 Therefore, the torn ACL is generally replaced by a substitute graft made of tendon.
he grafts commonly used to replace the ACL include:
- Patellar tendon autograft (autograft comes from the patient)
- Hamstring tendon autograft
- Quadriceps tendon autograft
- Allograft (taken from a cadaver) patellar tendon, Achilles tendon, semitendinosus, gracilis, or posterior tibialis tendon
Patients treated with surgical reconstruction of the ACL have long-term success rates of 82 percent to 95 percent. Recurrent instability and graft failure are seen in approximately 8 percent of patients.
The goal of the ACL reconstruction surgery is to prevent instability and restore the function of the torn ligament, creating a stable knee. This allows the patient to return to sports. There are certain factors that the patient must consider when deciding for or against ACL surgery.
Patient Considerations
Active adult patients involved in sports or jobs that require pivoting, turning or hard-cutting as well as heavy manual work are encouraged to consider surgical treatment.40, 41, 42, 43, 44 This includes older patients who have previously been excluded from consideration for ACL surgery. Activity, not age, should determine if surgical intervention should be considered.
In young children or adolescents with ACL tears, early ACL reconstruction creates a possible risk of growth plate injury, leading to bone growth problems. The surgeon can delay ACL surgery until the child is closer to skeletal maturity or the surgeon may modify the ACL surgery technique to decrease the risk of growth plate injury.45, 46
A patient with a torn ACL and significant functional instability has a high risk of developing secondary knee damage and should therefore consider ACL reconstruction.
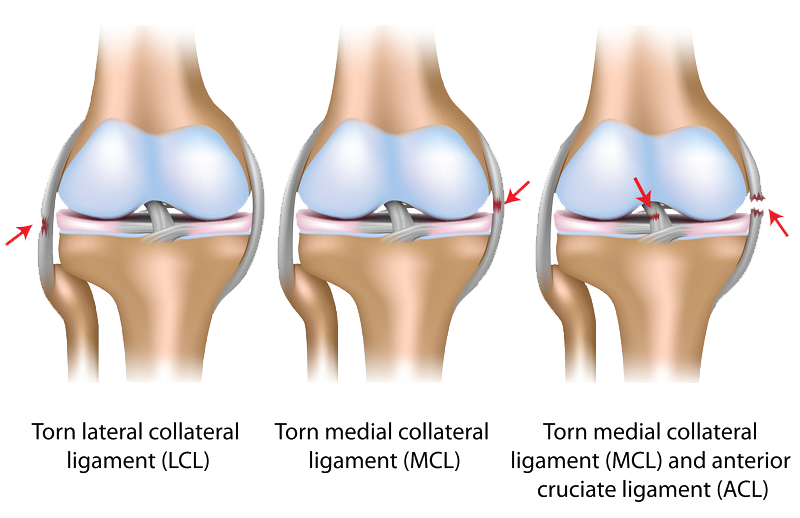
It is common to see ACL injuries combined with damage to the menisci (50 percent), articular cartilage (30 percent), collateral ligaments (30 percent), joint capsule, or a combination of the above. The “unhappy triad,” frequently seen in football players and skiers, consists of injuries to the ACL, the MCL, and the medial meniscus.23, 24, 25, 26, 27, 28, 29, 30, 31, 32
In cases of combined injuries, surgical treatment may be warranted and generally produces better outcomes.47, 48, 49, 50, 51, 52, 53, 54 As many as 50 percent of meniscus tears may be repairable and may heal better if the repair is done in combination with the ACL reconstruction.42, 55, 56
Surgical Choices
Patellar tendon autograft. The middle third of the patellar tendon of the patient, along with a bone plug from the shin and the kneecap is used in the patellar tendon autograft. Occasionally referred to by some surgeons as the “gold standard” for ACL reconstruction, it is often recommended for high-demand athletes and patients whose jobs do not require a significant amount of kneeling.57

In studies comparing outcomes of patellar tendon and hamstring autograft ACL reconstruction, the rate of graft failure was lower in the patellar tendon group (1.9 percent versus 4.9 percent).58 In addition, most studies show equal or better outcomes in terms of postoperative tests for knee laxity (Lachman’s, anterior drawer and instrumented tests) when this graft is compared to others. However, patellar tendon autografts have a greater incidence of postoperative patellofemoral pain (pain behind the kneecap) complaints and other problems.58,59
The pitfalls of the patellar tendon autograft are:
- Postoperative pain behind the kneecap
- Pain with kneeling
- Slightly increased risk of postoperative stiffness
- Low risk of patella fracture
Hamstring tendon autograft. The semitendinosus hamstring tendon on the inner side of the knee is used in creating the hamstring tendon autograft for ACL reconstruction. Some surgeons use an additional tendon, the gracilis, which is attached below the knee in the same area. This creates a two- or four-strand tendon graft. Hamstring graft proponents claim there are fewer problems associated with harvesting of the graft compared to the patellar tendon autograft including:
- Fewer problems with anterior knee pain or kneecap pain after surgery
- Less postoperative stiffness problems
- Smaller incision
- Faster recovery60, 61
The graft function may be limited by the strength and type of fixation in the bone tunnels, as the graft does not have bone plugs.62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73 There have been conflicting results in research studies as to whether hamstring grafts are slightly more susceptible to graft elongation (stretching), which may lead to increased laxity during objective testing.57, 58, 60, 61,74, 75, 76, 77, 78 Recently, some studies have demonstrated decreased hamstring strength in patients after surgery.79, 80, 81
There are some indications that patients who have intrinsic ligamentous laxity and knee hyperextension of 10 degrees or more may have increased risk of postoperative hamstring graft laxity on clinical exam. Therefore, some clinicians recommend the use of patellar tendon autografts in these hypermobile patients.130
Additionally, since the medial hamstrings often provide dynamic support against valgus stress and instability, some surgeons feel that chronic or residual medial collateral ligament laxity (grade 2 or more) at the time of ACL reconstruction may be a contra-indication for use of the patient’s own semitendinosus and gracilis tendons as an ACL graft.
Quadriceps tendon autograft. The quadriceps tendon autograft is often used for patients who have already failed ACL reconstruction.43, 82, 83 The middle third of the patient’s quadriceps tendon and a bone plug from the upper end of the knee cap are used. This yields a larger graft for taller and heavier patients. Because there is a bone plug on one side only, the fixation is not as solid as for the patellar tendon graft. There is a high association with postoperative anterior knee pain and a low risk of patella fracture. Patients may find the incision is not cosmetically appealing.
Allografts. Allografts are grafts taken from cadavers and are becoming increasingly popular.84, 85 These grafts are also used for patients who have failed ACL reconstruction before and in surgery to repair or reconstruct more than one knee ligament. Advantages of using allograft tissue include elimination of pain caused by obtaining the graft from the patient, decreased surgery time and smaller incisions. The patellar tendon allograft allows for strong bony fixation in the tibial and femoral bone tunnels with screws.

However, allografts are associated with a risk of infection, including viral transmission (HIV and Hepatitis C), despite careful screening and processing.86, 87, 88, 89 Several deaths linked to bacterial infection from allograft tissue (due to improper procurement and sterilization techniques) have led to improvements in allograft tissue testing and processing techniques.90 There have also been conflicting results in research studies as to whether allografts are slightly more susceptible to graft elongation (stretching), which may lead to increased laxity during testing.84, 91, 92, 93, 94
Recently published literature may point to a higher failure rate with the use of allografts for ACL reconstruction. Failure rates ranging from 23% to 34.4% have been reported in young, active patients returning to high-demand sporting activities after ACL reconstruction with allografts. This is compared to autograft failure rates ranging from 5% to 10%.131, 132, 133
The reason for this higher failure rate is unclear. It could be due to graft material properties (sterilization processes used, graft donor age, storage of the graft). It could possibly be due to an ill-advised earlier return to sport by the athlete because of a faster perceived physiologic recovery, when the graft is not biologically ready to be loaded and stressed during sporting activities. Further research in this area is indicated and is ongoing.
Surgical Procedure
Before any surgical treatment, the patient is usually sent to physical therapy. Patients who have a stiff, swollen knee lacking full range of motion at the time of ACL surgery may have significant problems regaining motion after surgery.95, 96, 97 It usually takes three or more weeks from the time of injury to achieve full range of motion. It is also recommended that some ligament injuries be braced and allowed to heal prior to ACL surgery.52,53, 54, 98
The patient, the surgeon, and the anesthesiologist select the anesthesia used for surgery. Patients may benefit from an anesthetic block of the nerves of the leg to decrease postoperative pain.
The surgery usually begins with an examination of the patient’s knee while the patient is relaxed due the effects of anesthesia. This final examination is used to verify that the ACL is torn and also to check for looseness of other knee ligaments that may need to be repaired during surgery or addressed postoperatively.
If the physical exam strongly suggests the ACL is torn, the selected tendon is harvested (for an autograft) or thawed (for an allograft) and the graft is prepared to the correct size for the patient.
After the graft has been prepared, the surgeon places an arthroscope into the joint. Small (one-centimeter) incisions called portals are made in the front of the knee to insert the arthroscope and instruments and the surgeon examines the condition of the knee. Meniscus and cartilage injuries are trimmed or repaired and the torn ACL stump is then removed.
In the most common ACL reconstruction technique, bone tunnels are drilled into the tibia and the femur to place the ACL graft in almost the same position as the torn ACL. A long needle is then passed through the tunnel of the tibia, up through the femoral tunnel, and then out through the skin of the thigh. The sutures of the graft are placed through the eye of the needle and the graft is pulled into position up through the tibial tunnel and then up into the femoral tunnel. The graft is held under tension as it is fixed in place using interference screws, spiked washers, posts, or staples. The devices used to hold the graft in place are generally not removed.
Variations on this surgical technique include the “two-incision,” “over-the-top,” and “double-bundle” types of ACL reconstructions, which may be used because of the preference of the surgeon or special circumstances (revision ACL reconstruction, open growth plates).45, 99, 100
Before the surgery is complete, the surgeon will probe the graft to make sure it has good tension, verify that the knee has full range of motion and perform tests such as the Lachman’s test to assess graft stability. The skin is closed and dressings (and perhaps a postoperative brace and cold therapy device, depending on surgeon preference) are applied. The patient will usually go home on the same day of the surgery.
Pain Management
After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Rehabilitation
Physical therapy is a crucial part of successful ACL surgery, with exercises beginning immediately after the surgery. Much of the success of ACL reconstructive surgery depends on the patient’s dedication to rigorous physical therapy. With new surgical techniques and stronger graft fixation, current physical therapy uses an accelerated course of rehabilitation.95, 96, 109
Postoperative Course. In the first 10 to 14 days after surgery, the wound is kept clean and dry, and early emphasis is placed on regaining the ability to fully straighten the knee and restore quadriceps control.
The knee is iced regularly to reduce swelling and pain. The surgeon may dictate the use of a postoperative brace and the use of a machine to move the knee through its range of motion.124,125 Weight-bearing status (use of crutches to keep some or all of the patient’s weight off of the surgical leg) is also determined by physician preference, as well as other injuries addressed at the time of surgery.
Rehabilitation. The goals for rehabilitation of ACL reconstruction include reducing knee swelling, maintaining mobility of the kneecap to prevent anterior knee pain problems, regaining full range of motion of the knee, as well as strengthening the quadriceps and hamstring muscles.
The patient may return to sports when there is no longer pain or swelling, when full knee range of motion has been achieved, and when muscle strength, endurance and functional use of the leg have been fully restored.
The patient’s sense of balance and control of the leg must also be restored through exercises designed to improve neuromuscular control.4 This usually takes four to six months. The use of a functional brace when returning to sports is ideally not needed after a successful ACL reconstruction, but some patients may feel a greater sense of security by wearing one.126, 127,128, 129
Surgical Complications
Infection. The incidence of infection after arthroscopic ACL reconstruction has a reported range of 0.2 percent to 0.48 percent.101, 102, 103, 104 There have also been several reported deaths linked to bacterial infection from allograft tissue due to improper procurement and sterilization techniques.90
Viral transmission. Allografts specifically are associated with risk of viral transmission, including HIV and Hepatitis C, despite careful screening and processing.86, 87, 88, 89 The chance of obtaining a bone allograft from an HIV-infected donor is calculated to be less than 1 in a million.87
Bleeding, numbness. Rare risks include bleeding from acute injury to the popliteal artery (overall incidence is 0.01 percent) 105 and weakness or paralysis of the leg or foot. It is not uncommon to have numbness of the outer part of the upper leg next to the incision, which may be temporary or permanent.106, 107
Blood clot. A blood clot in the veins of the calf or thigh is a potentially life-threatening complication. A blood clot may break off in the bloodstream and travel to the lungs, causing pulmonary embolism or to the brain, causing stroke. This risk of is reported to be approximately 0.12 percent.
Instability. Recurrent instability due to rupture or stretching of the reconstructed ligament or poor surgical technique (reported to be as low as 2.5 percent and as high as 34 percent) is possible.2, 25, 58, 108, 131, 132, 133
Stiffness. Knee stiffness or loss of motion has been reported at between 5 percent and 25 percent.58, 109, 110, 111, 112, 113
Extensor mechanism failure. Rupture of the patellar tendon (patellar tendon autograft) or patella fracture (patellar tendon or quadriceps tendon autografts) may occur due to weakening at the site of graft harvest.114, 115, 116, 117, 118, 119, 120
Growth plate injury. In young children or adolescents with ACL tears, early ACL reconstruction creates a possible risk of growth plate injury, leading to bone growth problems.45, 46, 121, 122, 123The ACL surgery can be delayed until the child is closer to reaching skeletal maturity. Alternatively, the surgeon may be able to modify the technique of ACL reconstruction to decrease the risk of growth plate injury.
Kneecap pain. Postoperative anterior knee pain is especially common after patellar tendon autograft ACL reconstruction. The incidence of pain behind the kneecap varies between 4 percent and 56 percent in studies, whereas the incidence of kneeling pain may be as high as 42 percent after patellar tendon autograft ACL reconstruction.58
Anterior Cruciate Ligament Reconstruction (ACL Reconstruction)
The ACL is one of main ligaments in the knee (and one of the most commonly injured) and connects the femur to the tibia. Because the knee has a hinged joint that experiences constant movement and supports a lot of weight, damage to the ACL is common, particularly in athletes and may require reconstructive surgery.
How Does ACL reconstruction Work?
- ACL reconstruction aims to restore function to the knee after an injury to the anterior cruciate ligament.
- Because most ACL tears cannot be repaired, the torn ligament needs to be reconstructed. The torn ligament is removed and a graft is used in its place. New ligament will grow on the graft. We generally use graphs obtained from the patient’s body-usually from tendons.
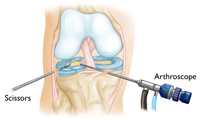
- The procedure is undertaken using arthroscopic surgery.
Knee Ligament Reconstruction
Ligaments that are badly damaged or ruptured need to be repaired through reconstructive surgery.
There are four major ligaments in the knee. The ligaments in the knee connect the femur (thighbone) to the tibia (shin bone), and include the following:
- Anterior cruciate ligament (ACL). The ligament, located in the center of the knee, that controls rotation and forward movement of the tibia (shin bone).
- Posterior cruciate ligament (PCL). The ligament, located in the center of the knee, that controls backward movement of the tibia.
- Medial collateral ligament (MCL). The ligament that gives stability to the inner knee.
- Lateral collateral ligament (LCL). The ligament that gives stability to the outer knee.
How Does Knee Ligament Reconstruction Work?
When your knee is severely damaged by injury or arthritis, even everyday activities can become painful and difficult. You may find walking up stairs very painful and even sitting or lying uncomfortable. If non-surgical interventions are not helpful, it may be time to consider knee replacement surgery.
Knee ligament reconstruction aims to restore function to the knee after an injury to the ligament has occurred. Also known as arthroplasty, this procedure aims to resurface the damaged knee. The replacement “knee” is made from metal and plastic, and caps off the ends of the bones that make up the knee joint as well as the kneecap. Partial knee replacement may be a suitable alternative to total knee replacement.
The doctor performs the surgery using an arthroscope (a small tube-shaped instrument that is inserted into a joint). The doctor may reattach the torn ligament or reconstruct the torn ligament by using a portion (graft) of the patellar tendon, the hamstring tendon, or other autografts. The tendon graft may come from the patient (autograft) or from an organ donor (allograft).
Knee Replacement Surgery
Knee replacement surgery takes place over four steps.
- Bone Preparation. The damaged cartilage at the ends of the femur and tibia are removed, in addition to some underlying bone.
- Metal Implants are Inserted. Metal components replace the damaged cartilage and bone, and recreate the surface of the joint.
- Patella Resurfacing. The patella (kneecap) is cut down and resurfaced with plastic. (Not all knee replacement requires this procedure).
- Spacer is Inserted. A surgical plastic spacer is inserted between the components to ensure a smooth surface.
Minimally Invasive Total Knee Replacement
The traditional approach to knee replacement uses a long vertical incision in the knee in order to access the joint and view it clearly. With minimally invasive total knee replacement, the surgeon uses a variation to this approach. The incision is shorter and the technique is less invasive. The outcome is usually less post-operative pain and faster recovery time.
The minimally invasive technique is not suitable for all patients, so it’s important you make an appointment to discuss your suitability with Dr. Sima.
Revision Total Knee Replacement
While many patients need no further intervention, it’s possible that gradually a knee replacement may fail. If this happens, your knee may feel swollen and painful. The joint may also be feeling stiff or unstable, and everyday tasks may become more difficult.
If this occurs, your doctor may suggest a further procedure, known as revision total knee replacement, where most or all of the previous prosthetic parts are removed and replaced.
Revision Total Knee Replacement Surgery is a complicated procedure that requires more sophisticated tools and extensive planning in order to achieve a desirable result. Feel free to contact us for further information on this procedure, by calling our office on
Partial Knee Reconstruction (Unicompartmental Knee Replacement)
Partial knee replacement is a surgical treatment option that replaces (or resurfaces) only the damaged portion of the knee while conserving knee ligaments and unaffected cartilage. Unicompartmental knee replacement is a common treatment for osteoarthritis.
With knee osteoarthritis, the cartilage protecting the bones of the knee slowly deteriorates and wears away. The whole knee joint may be affected, or just a single region of the knee.
The three compartments of the knee are as follows:
- Medial compartment (the inside part of the knee)
- Lateral compartment (the outside part)
- Patellofemoral compartment (the front of the knee between the kneecap and thighbone)
If your Osteoarthritis is limited to a single compartment of the knee, it may be treatable with a unicompartmental knee replacement.
Iovera° Treatment
If your knee pain is chronic, due to osteoarthritis, it can be alleviated by cryoanalgesia with the iovera° treatment. The iovera° system has also been shown to help in reducing opioid consumption in patients after surgery. Postsurgical pain is considered to be acute pain.
The iovera° treatment is a focused therapy; therefore, there are no side effects to the entire body. Nothing is injected into the treatment area by the iovera° system. Therefore, very few, if any, localized side effects due to the iovera° treatment have been observed and side effects are mild.
Advantages of Partial Knee Replacement
The advantages of unicompartmental replacement over total knee replacement include:
- faster recovery time
- minimized blood loss
- minimized post-operative pain
- more natural, as the cartilage, ligaments, and healthy bone are all retained.
It’s important to note that in some cases total knee replacement surgery may still be necessary in the future, especially if the original parts of the knee that were not replaced develop arthritic symptoms. Of course, it’s best to make an appointment with Dr. Sima to put your mind at ease and discuss your options.
The Subchondroplasty® (SCP®) Procedure
Subchondroplasty (SCP) is a procedure designed to correct bone marrow lesions-a cause of osteoarthritis– using state-of-the-art bone substitute material (BSM) made from calcium phosphate.
The SCP Procedure is usually performed in conjunction with arthroscopy. In some cases, an open procedure is necessary to determine the defect.
Knee osteoarthritis, a progressive disease that causes joint cartilage to wear away over time, can often benefit from SCP.
Who is Suitable for the (SCP) Procedure Suitable?
Patients who have been diagnosed with bone marrow lesions will generally benefit the most from SCP.
How is SCP Performed?
- Subchondroplasty is a procedure performed to locate and target bone marrow lesions. An MRI will usually take place prior to the surgery.
- The patient is administered a general anesthetic
- A small frame is placed in-line with the patient’s tibia to help the surgeon target the exact location of the lesion.
- A pin is inserted into the patient’s skin, through to the bone.
- The pin is inserted into the bone at the appropriate depth and the guide is removed.
- The semi-circular guide is then removed, leaving only the pin.
- Next, a cannula is placed over the pin and is slid into the bone until it is firmly in place. A syringe filled with the bone substitute is attached to the cannula
- Finally, the bone substitute is injected gently into the bone.
What to Expect After Surgery
For a few days after the procedure it’s normal to feel some pain and discomfort. The symptoms can usually be treated with simple pain medications.
Gentle exercises may also be encouraged.
Microfracture
The goal of microfracture is to stimulate the growth of new articular cartilage by creating a new blood supply. A sharp tool called an awl is used to make multiple holes in the joint surface. The holes are made in the bone beneath the cartilage, called subchondral bone. This action creates a healing response. New blood supply can reach the joint surface, bringing with it new cells that will form the new cartilage.
The goal of microfracture is to stimulate the growth of new cartilage by creating a new blood supply.
Juvenile Cartilage Transplant
DeNovo® NT Natural Tissue Graft is an off-the-shelf human tissue, consisting of viable, juvenile hyaline cartilage pieces and is intended for the repair of articular cartilage defects in a single-stage procedure. The DeNovo NT Graft surgical technique mitigates the need for harvesting and suturing of a periosteal flap, unlike autologous chondrocyte implantation (ACI), as it employs a fibrin sealant to secure the minced tissue pieces into the defect.
Meniscal Tears
Meniscus tears are among the most common knee injuries. Athletes, particularly those who play contact sports, are at risk for meniscus tears. However, anyone at any age can tear a meniscus. When people talk about torn cartilage in the knee, they are usually referring to a torn meniscus.
Anatomy
Three bones meet to form your knee joint: your thighbone (femur), shinbone (tibia), and kneecap (patella).
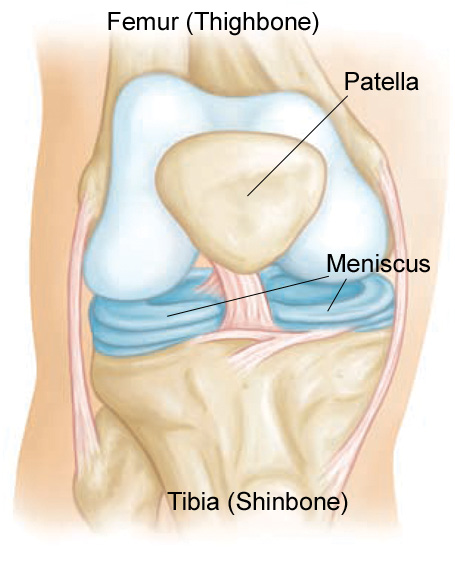
Two wedge-shaped pieces of cartilage act as “shock absorbers” between your thighbone and shinbone. These are called meniscus. They are tough and rubbery to help cushion the joint and keep it stable.
Description
Menisci tear in different ways. Tears are noted by how they look, as well as where the tear occurs in the meniscus. Common tears include bucket handle, flap, and radial.

Sports-related meniscus tears often occur along with other knee injuries, such as anterior cruciate ligament tears.
Cause
Sudden meniscus tears often happen during sports. Players may squat and twist the knee, causing a tear. Direct contact, like a tackle, is sometimes involved.
Older people are more likely to have degenerative meniscus tears. Cartilage weakens and wears thin over time. Aged, worn tissue is more prone to tears. Just an awkward twist when getting up from a chair may be enough to cause a tear, if the menisci have weakened with age.
Symptoms
You might feel a “pop” when you tear a meniscus. Most people can still walk on their injured knee. Many athletes keep playing with a tear. Over 2 to 3 days, your knee will gradually become more stiff and swollen.
The most common symptoms of meniscus tear are:
- Pain
- Stiffness and swelling
- Catching or locking of your knee
- The sensation of your knee “giving way”
- You are not able to move your knee through its full range of motion
Without treatment, a piece of meniscus may come loose and drift into the joint. This can cause your knee to slip, pop, or lock.
Doctor Examination
After discussing your symptoms and medical history, your doctor will examine your knee. He or she will check for tenderness along the joint line where the meniscus sits. This often signals a tear.
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement will cause a clicking sound. Your knee will click each time your doctor does the test.
Imaging Tests
Because other knee problems cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. Although x-rays do not show meniscus tears, they may show other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI). This study can create better images of the soft tissues of your knee joint, like a meniscus.
Treatment
How your orthopaedic surgeon treats your tear will depend on the type of tear you have, its size, and location.
The outside one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a blood supply. Without nutrients from blood, tears in this “white” zone cannot heal. These complex tears are often in thin, worn cartilage. Because the pieces cannot grow back together, tears in this zone are usually surgically trimmed away.
Along with the type of tear you have, your age, activity level, and any related injuries will factor into your treatment plan.
Nonsurgical Treatment
If your tear is small and on the outer edge of the meniscus, it may not require surgical repair. As long as your symptoms do not persist and your knee is stable, nonsurgical treatment may be all you need.
RICE. The RICE protocol is effective for most sports-related injuries. RICE stands for Rest, Ice, Compression, and Elevation.
- Rest. Take a break from the activity that caused the injury. Your doctor may recommend that you use crutches to avoid putting weight on your leg.
- Ice. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly to the skin.
- Compression. To prevent additional swelling and blood loss, wear an elastic compression bandage.
- Elevation. To reduce swelling, recline when you rest, and put your leg up higher than your heart.
- Non-steroidal anti-inflammatory medicines. Drugs like aspirin and ibuprofen reduce pain and swelling.
Surgical Treatment
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In it, a miniature camera is inserted through a small incision (portal). This provides a clear view of the inside of the knee. Your orthopaedic surgeon inserts miniature surgical instruments through other portals to trim or repair the tear.
- Partial meniscectomy. In this procedure, the damaged meniscus tissue is trimmed away.
- Meniscus repair. Some meniscus tears can be repaired by suturing (stitching) the torn pieces together. Whether a tear can be successfully treated with repair depends upon the type of tear, as well as the overall condition of the injured meniscus. Because the meniscus must heal back together, recovery time for a repair is much longer than from a meniscectomy.
Rehabilitation. After surgery, your doctor may put your knee in a cast or brace to keep it from moving. If you have had a meniscus repair procedure, you will need to use crutches for about a month to keep weight off of your knee.
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
For the most part, rehabilitation can be carried out at home, although your doctor may recommend physical therapy. Rehabilitation time for a meniscus repair is about 3 months. A meniscectomy requires less time for healing — approximately 3 to 4 weeks.
Recovery
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
My knee was bent and I could not straighten it because of a sports injury. But then, you operated on me and when I awoke, all the pain was gone. After a brief recovery, I could, once more walk and run as I did before my injury. I have a tiny scar on my knee. Your skilled hands performed what amounts to a miracle in my life and I have been grateful to you every day since that time.
-Marcia Triggs
Non-Surgical Knee Procedures
Many surgery alternatives are available for those whose injuries and conditions can still be treated without requiring surgical intervention. Please explore these options below and contact our office to book your appointment and discuss your situation.
What is Mesenchymal Progenitor Cell (MPC) Therapy?
Your body consists of billions of cells that degenerate and regenerate in a daily cycle. As older cells die off, new cells are created from the stem cells. The cells form organs of the body such as skin, muscles, ligaments, joints, bone, tendons and the brain. Unfortunately, if tissue is damaged, the degenerative process dominates the cycle and the organs will become less functional, and pain will often result. The stem cells used for MSC are found in your own bone marrow and are known as mesenchymal cells.
Which Conditions Benefit from MSC Therapy?
Degenerative conditions such as osteoarthritis and joint injuries respond well to MSC therapy. Contact our office to find out whether you are a candidate for this advanced procedure
How Does it Work?
- Stem cells are obtained from the patient’s body, generally from within the bone marrow of the hip area.
- The procedure takes place in our clinic, under ultrasound or x-ray guidance
- You will lie face down and the doctor will thoroughly clean the area. Next, a needle penetrates the bone and will remove blood from within the marrow, which contains the stem cells.
- After the procedure, the stem cell rich blood is taken to the laboratory where it is concentrated, cells that are not required are removed, and the remaining stem cells purified.
- The stem cells are injected precisely by hand into the injured tissues in other areas of the body using MSK Ultrasound for guidance. Through imaging devices, your doctor can ensure the cells are injected precisely at the site of need.
Once the stem cells are injected, they will enhance the natural repair process of degenerated and injured tendons, ligaments, and arthritic joints.
Platelet-rich Plasma (PRP) Treatment
Platelet-Rich Plasma Treatment, also known as PRP, is a popular treatment method for a variety of knee problems. It is often used by athletes due to its lack of negative side effects and the fact that little recovery time needed after the procedure.
What is PRP?
Though our blood seems to be all liquid (which is called plasma), it contains very small solid parts such as red cells, white cells, and platelets. Platelets play an important role in helping blood to clot, and platelets also contain growth factors that help the body heal itself.
How Does PRP Work?
First, blood is removed from the patient. Platelets are separated and removed from the other blood components through a process known as centrifugation. The increased concentration of growth factors in PRP speed up the body’s healing process. PRP is gently injected into the site of the injury. PRP can also be used to aid in healing after surgery for some injuries.
What Conditions Benefit from PRP?
A number of conditions may benefit from PRP treatment, but it is important to visit our office to determine whether your unique condition will be suitable for this treatment.
Some common problems that have been successfully treated by PRP include:
- Chronic and acute tendon injuries
- Acute Ligament and Muscle Injuries
- Arthritis
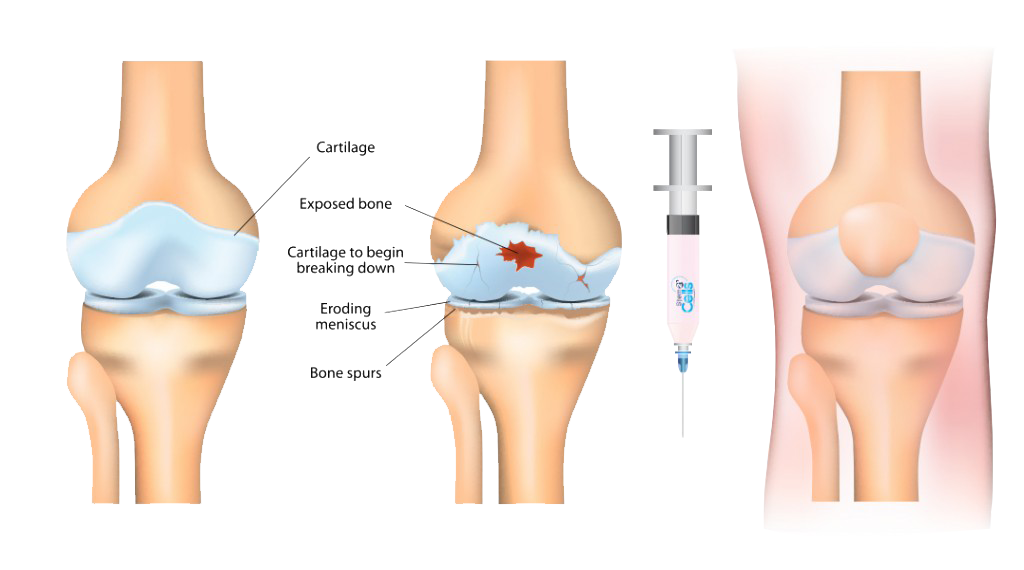
Iovera° Treatment
If your knee pain is chronic, due to osteoarthritis, it can be alleviated by cryoanalgesia with the iovera° treatment. The iovera° system has also been shown to help in reducing opioid consumption in patients after surgery. Postsurgical pain is considered to be acute pain.
The iovera° treatment is a focused therapy; therefore, there are no side effects to the entire body. Nothing is injected into the treatment area by the iovera° system. Therefore, very few, if any, localized side effects due to the iovera° treatment have been observed and side effects are mild.