We are very excited to now offer outpatient anterior total hip replacement surgery, total knee replacement surgery, shoulder replacement surgery,and unicompartmental knee replacement to select patients. These procedures represents the next trend in arthroplasty surgery. Many surgeries done today as outpatient procedures were once regarded as “inpatient” procedures. These include ACL reconstruction, rotator cuff repair, upper extremity surgery and arthroscopy. Just a decade ago, a cholecystectomy (gallbladder removal) was performed as an inpatient procedure. Improvements in surgical techniques and anesthesia protocols have allowed surgeons to safely perform these operations in a dedicated surgical suite where patients can safely return home the same day as their procedure. Patient selection, medical optimization and perioperative care and planning are essential.
Further Reading
Aynardi et al., HSS J 2014.
Cross MB, Berger R. Feasibility and safety of performing outpatient unicompartmental knee arthroplasty. Int Orthop. 2014 Feb;38(2):4437.
Gondusky JS, Choi L, Khalaf N, Patel J, Barnett S, Gorab R. Day of surgery discharge after unicompartmental knee arthroplasty: an effective perioperative pathway. J Arthroplasty. 2014 Mar;29(3):5169.
Berger RA, Kusuma SK, Sanders SA, Thill ES, Sporer SM. The feasibility and perioperative complications of outpatient knee arthroplasty, Clin Orthop Relat Res. 2009 Jun;467(6):14439.
Larsen K, Hansen TB, Soballe K, Kehlet H. Patient reported outcome after fasttrack knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012 Jun;20(6):112835.
Adipose-derived Progenitor Cells
The Lipogems procedure uses cutting-edge technology that gently processes your body’s own fat tissue in order to, amongst other things, cushion and support areas of injury or damage as your body heals itself. Lipogems is injected precisely into areas of the body in order to help establish an environment conducive to tissue healing and repair. Lipogems tends to stay in the area where it is injected instead of being reabsorbed by the body, allowing your body to maximize the benefits of Lipogems for an extended period of time. As part of this overall process, Lipogems provides cushioning and structural support to your body’s tissues wherever it is injected.
For more information visit http://www.understandlipogems.com/

Autologous Platelet Rich Plasma (PRP)
These therapies have become increasingly popular within the field of orthopaedics over the past 5 years. PRP is defined as “a volume of plasma that has a platelet count above baseline of whole blood.” PRP contains many growth factors important in tissue healing and regeneration. Current applications supported by recent literature show evidence for use of PRP in lateral epicondylitis (tennis elbow), patellar tendonitis, arthritis, and muscle injuries.
Further Reading
Hsu et al. “Plateletrich Plasma in Orthopaedic Applications: Evidencebased Recommendations for Treatment”, JAAOS December 2013

Autologous Protein Solution: Intra-Articular Injection for the Treatment of Early OA
APS processes your own blood to provide a true novel output. The unique output is injected directly into the knee joint distributing beneficial and good proteins. In laboratory testing, these “good” proteins block and slow the degradation of cartilage treating the underlying cause of OA knee pain, unlike traditional therapies.
• Significantly reduces pain associated with Knee OA.
• Significantly improves Mobility in the Knee Joint associated with OA
• Stimulates Cartilage Cell Proliferation.
• Blocks Cartilage Destruction.
• Slows Cartilage Degradation.
• Single injection
Further Reading
http://www.pressreader.com/…/the-s…/20160904/282832190552479

Mesenchymal Progenitor Cells (MPCs)
MSCs are multipotent cells found in the bone marrow that have the ability to differentiate into bone, cartilage, muscle and other mesenchymal tissue. MSCs are antiinflammatory, immunomodulatory, and enhance the formation of organized tissue. These cells are often isolated from the superior iliac crest, but alternative donor sites including the femur and tibia can also be used. Potential areas of use include bone healing, tendinopathy, cartilage regeneration, arthritis, ligament and tendon repair, and muscle regeneration.
Further Reading
Tuan RS, Chen AF, Klatt BA. Cartilage regeneration. J Am Acad Orthop Surg. 2013 May;9(5):30311. Review.PMID: 23591485
Autologous Chondrocyte Implantation (ACI)
ACI is a two-step procedure. New cartilage cells are grown and then implanted in the cartilage defect. First, healthy cartilage tissue is removed from a non-weight bearing area of the bone. This step is done as an arthroscopic procedure. The tissue which contains healthy cartilage cells, or chondrocytes, is then sent to the laboratory. The cells are cultured and increase in number over a 3- to 5-week period. An open surgical procedure, or arthrotomy, is then done to implant the newly grown cells. The cartilage defect is prepared. A layer of bone-lining tissue, called periosteum, is sewn over the area. This cover is sealed with fibrin glue. The newly grown cells are then injected into the defect under the periosteal cover. ACI is most useful for younger patients who have single defects larger than 2 cm in diameter. ACI has the advantage of using the patient’s own cells, so there is no danger of a patient rejecting the tissue. It does have the disadvantage of being a two-stage procedure that requires an open incision. It also takes several weeks to complete.
Further Reading

Osteoarticular Transfer System
Commonly known as OATS, this procedure replaces damaged cartilage in the knee with healthy cartilage from another area of the joint, relieving pain and restoring movement and function to the joint. A mosaicplasty is the name for a general procedure that treats severe cartilage damage, and the OATS procedure is one type of mosaicplasty. Although cartilage is essential to smooth, painless movement of the joints, some areas have a more critical need for the support and cushioning provided by the cartilage. During the OATS procedure, small plugs of healthy cartilage are removed from areas of the joint that are not in critical need and transferred to the area of damaged cartilage.
The OATS procedure is ideal for patients with small areas of cartilage damage that can be easily repaired with a graft. Widespread cartilage damage cannot usually be treated with this procedure, since there may be insufficient amounts of healthy cartilage available. After the OATS procedure, patients will need to undergo a lengthy physical therapy program in order to restore range of motion and relieve pain and swelling on the joint. Most patients will be on crutches for 6 to 12 weeks after surgery before they can successfully bear weight on the joint again. Long-term follow-up care will be required in order to maintain the results of this procedure.
Further Reading
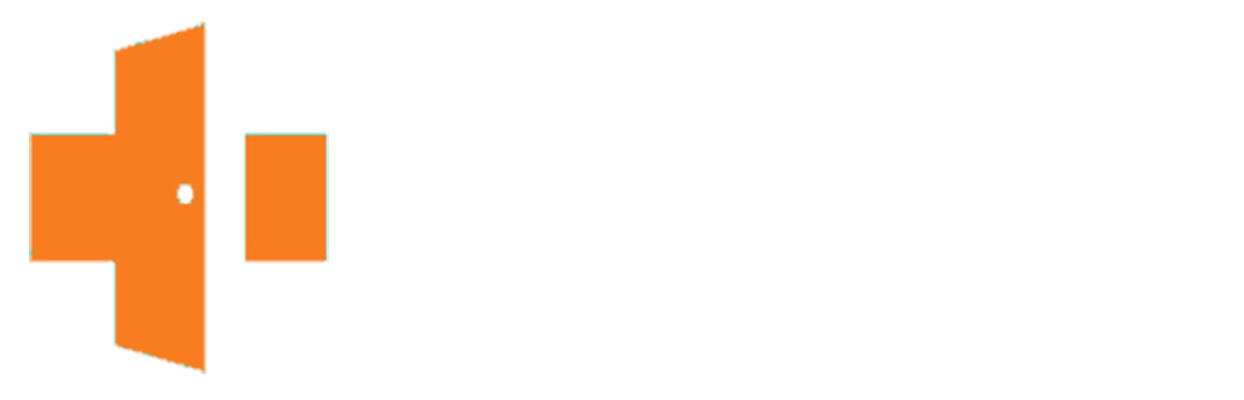
The Anterior Approach
This approach to hip replacement surgery allows the surgeon to reach the hip joint from the front of the hip as opposed to the lateral (side) or the posterior (back) approach. This way, the hip can be replaced without detachment of muscle from the pelvis or femur during surgery.
Further Information
Learn more about anterior hip replacement here
View anterior hip replacement videos
Newhipnews.com: Dedicated to Anterior Hip Replacement
New Study on Total Hip Arthroplasty with Anterior Approach
Subchondroplasty (SCP)
SCP is a minimally invasive treatment for defects in bone called bone marrow lesions. Bone marrow lesions represent the healing response to areas of insufficiency and micro fractures known to cause joint pain and accelerate joint damage. These lesions are often found within the knee joints. Bone marrow lesions can be diagnosed using magnetic resonance imaging (MRI). SCP treats bone marrow lesions in the knee joint by filling in the defects with an absorbable material. This material is then eventually resorbed and replaced with healthy bone. This procedure can be performed in 30-60 minutes in an out patient surgery center and patients can return home the same day of their surgery.
Further Reading
Unicompartmental knee replacement or partial knee replacement
This is a surgical procedure where only the damaged portion of the knee is replaced. There are three compartments of the knee. Depending on if your arthritis is confined to a single compartment of your knee will dictate whether you may be a good candidate. Advantages of the unicompartmental knee replacement are quicker recovery, less pain after surgery, and less blood loss. In some cases, a unicompartmental knee replacement can be performed in an outpatient surgical suite and patients can return home the same day of their surgery.
Further Reading

SpeedBridge Technique
This is a knotless technique for the repair of a rotator cuff tear that creates a quick and secure construct with no knots that maximizes contact between tendon and bone to enhance healing.