Shoulder Surgery
Surgery & Surgery Alternatives
Shoulder surgery may be the best option for your shoulder injury, but there are surgery alternatives as well. We offer the latest in medical advancement to ensure that we find the best treatment for your injury or condition. Review shoulder surgery and surgery alternative options, success rates, recovery times and more below.
Surgical Shoulder Procedures
Rotator Cuff Repair
Your doctor may recommend different treatment options depending on your particular symptoms and the severity of your condition.
Rest up. Your doctor will likely recommend that you avoid engaging in any activity that causes symptoms or makes your symptoms feel worse. That may mean the temporary use of a sling.
Manage the pain. Your doctor may prescribe or recommend the use of anti-inflammatory medications (like aspirin or ibuprofen) and ice packs applied to the shoulder to reduce inflammation and pain. Often a local injection of cortisone or lidocaine, or both, helps to further reduce inflammation.
Get the right moves. Your doctor may recommend several specific strengthening exercises for you to perform on your own throughout the day. You may even be given a prescription for a course of physical therapy. During physical therapy sessions, a trained therapist may apply heat wraps, use painless electro-stimulation, provide massage and/or teach you special exercises to help reduce your pain, increase your motion and improve your strength.
Understand your surgical options. If you are still experiencing pain after all other conservative measures have been taken, or if your tear is the result of a traumatic injury, your doctor may suggest surgery to repair the tear, help relieve your pain and help restore your mobility. Surgical procedures to repair a rotator cuff tear range from debriding (a procedure in which a partial tear is smoothed) to stitching the torn tendon and, if necessary, re-attaching it to the humerus bone with small anchors. Your doctor will help you to determine the procedure most appropriate for you and for the extent of your injury.
Today’s techniques, matched with newer instruments, may allow your doctor to repair your rotator cuff tear on an outpatient basis with mini-open surgery (requiring only a two- to three-inch incision) or arthroscopic surgery (using a fiber optic scope, requiring even smaller incisions). To secure your repair, your doctor will use anchor options that are designed to meet the needs of your injury, your anatomy and your doctor’s preference, including both titanium and “bioabsorbable” anchors. Bioabsorbables are designed to allow the body to use the anchor as a scaffold to build its own permanent repair.
Be sure to talk with your doctor about the best treatment option for you.
Commit to feeling better. Whether your doctor performs mini-open surgery, or even less-invasive arthroscopic surgery, you will likely be able to go home the same day. You may have to keep your arm in a sling for a period of time while you heal. Although full recovery from rotator cuff injury and repair may take several months, during that time you will be engaged in specific exercises, perhaps a course of rehabilitative physical therapy, to help regain your full range of motion without pain. Complete rehabilitation often depends on your commitment to following your doctor’s recovery recommendations. Your doctor can also help you determine how soon after surgery you can safely begin participating in activities that involve the rotator cuff.
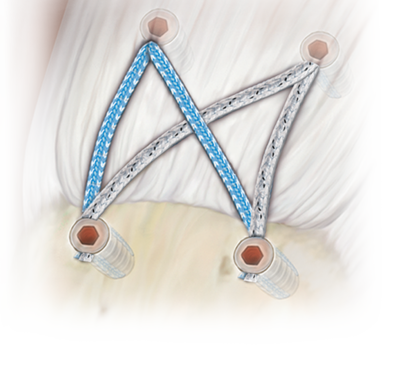
The SpeedBridge™ Knotless Technique
The SpeedBridge™ Knotless Technique is used to repair rotator cuff tears and includes a fully threaded SwiveLock® anchor combined with FiberTape® to create a quick and secure construct with no knots and only two suture passing steps. The result is a low profile, transosseous-equivalent “SutureBridge” that enhances footprint compression to maximize contact between tendon and bone. The SpeedBridge utilizes FiberTape which provides three times the contact area compared to a standard #2 FiberWire®. It provides a broad footprint which can be helpful for repairs in degenerative cuff tissue where tissue pull-through may be a concern.
Stryker InSpace Balloon
The Stryker InSpace Balloon is used to treat massive irreparable rotator cuff tears. The InSpace biodegradable implantable balloon system includes an introducer and a pre-shaped balloon spacer made of a biodegradable copolymer that biodegrades over the course of 12 months. The implant is designed to restore the subacromial space without the need for sutures, fixation devices or any kind of discomfort. It is claimed to be able to improve shoulder mobility and function. The balloon is inserted using a cylinder-shaped insertion tube, which is withdrawn once the spacer is placed into the subacromial space. It is implanted, either arthroscopically or via a five-step mini-open surgery, between the acromion and the humeral head or rotator cuff. It creates a space between the bone structures, allowing the humeral head to glide smoothly or frictionless against the acromion.
Dr. Sima can advise you whether or not the SpeedBridge Technique or InSpace Balloon is right for your specific condition.

Labral/SLAP Repair
A SLAP lesion, (which stands for a tear in the Superior Labrum, Anterior to Posterior) is where the labrum is torn from the front to the back. Sudden pulls on the muscle can pull the superior labrum off the bone.
Shoulder SLAP Repair
SLAP repair is performed using arthroscopic surgery. Under general anesthetic and a nerve block, the torn labrum is reattached using sutures and small bone anchors. Following surgery the patient will need to wear a sling.
The end result is generally very favorable and we encourage you to contact Dr. Sima to find out whether SLAP repair is right for you.
Subacromial Decompression
The goal of this surgery is to create more space for the rotator cuff. To do this, your doctor will remove the inflamed portion of the bursa. The doctor may also perform an anterior acromioplasty, a procedure to remove part of the acromion. This is also known as a subacromial decompression. These procedures can be performed using either an arthroscopic or open technique.
Arthroscopic technique. In arthroscopy, thin surgical instruments are inserted into two or three small puncture wounds around your shoulder. Your doctor examines your shoulder through a fiberoptic scope connected to a television camera. He or she guides the small instruments using a video monitor, and removes bone and soft tissue. In most cases, the front edge of the acromion is removed along with some of the bursal tissue.
Your surgeon may also treat other conditions present in the shoulder at the time of surgery. These can include arthritis between the clavicle (collarbone) and the acromion (acromioclavicular arthritis), inflammation of the biceps tendon (biceps tendonitis), or a partial rotator cuff tear.
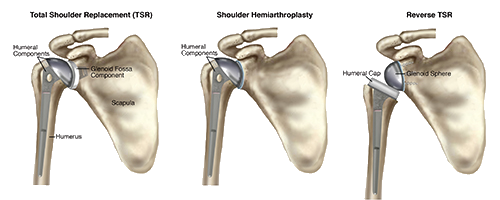
Total Shoulder Replacement
Shoulder joint replacement is a procedure similar to a knee or hip replacement, aiming to alleviate pain and help the patient to undertake normal daily activities without difficultly.
Shoulder replacement is a very common surgery and is reserved for painful conditions of the shoulder, including arthritis, that hasn’t responded to non-surgical interventions. Total replacement surgery is very safe and generally has excellent results.
In shoulder replacement surgery, the parts of the shoulder that are not functioning well are removed and replaced with prosthetic components. Total shoulder replacement includes both the humerus (ball) and glenoid (socket). Occasionally only the humerus bone needs replacement.
Click here for more information on shoulder replacement surgery.
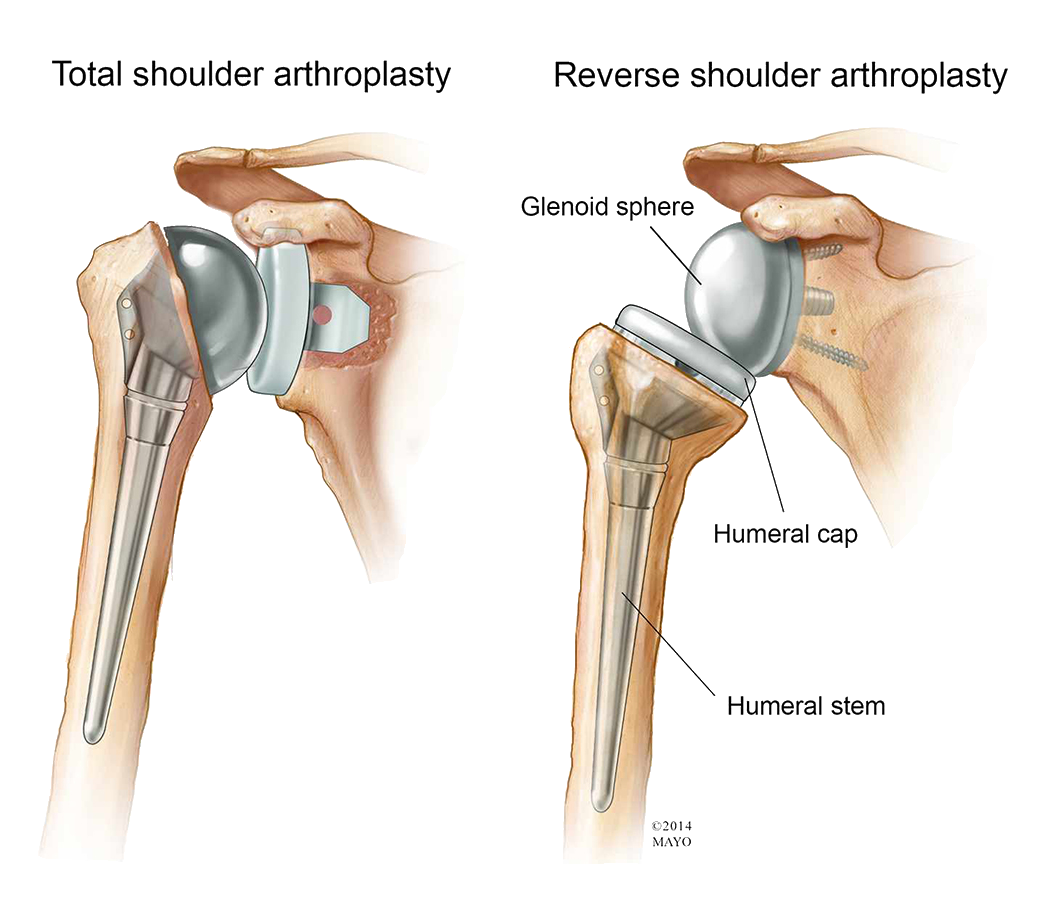
Reverse Total Shoulder Replacement
Reverse shoulder replacement is a variation of total shoulder replacement, used for patients who have:
- Previous shoulder replacement surgery that has failed
- Severe arm weakness
- Completely torn rotator cuffs
- Severe rotator cuff tearing and severe arthritis
In reverse total shoulder replacement, the socket and metal ball are attached differently. The metal ball is attached to the shoulder bone, and a plastic socket is attached to the upper arm bone.
Following shoulder replacement surgery, the patient generally starts a physical therapy program. Such a program will help improve flexibility and strengthen the shoulder.
Superior Capsular Reconstruction (SCR)
Tears to the rotator cuff are common in young and active people and are most often repaired with surgery. Tears have not been diagnosed get damaged more and more over time. Scarring can occur in these instances, and muscles can even atrophy. This condition can be quite painful, as without a functioning rotator cuff, the deltoid cannot pull against a fulcrum. As a result, when the deltoid contracts to lift the arm, the humerus elevates instead and hits against the upper shoulder blade.
Older patients with the same problem are often treated with reverse shoulder arthroplasty (RSA), but these devices were not invented for long-term use or heavy use by younger people, therefore RSA is not common for those under 50.
In 2007, a Japanese surgeon developed SCR as an surgery option for younger people. Like the RSA, this procedure changed the way the shoulder operates. The deltoid can lift the arm irrespective of the absent rotator cuff. However, unlike the RSA, SCR does not replace any part of the joint.
How Does it Work?

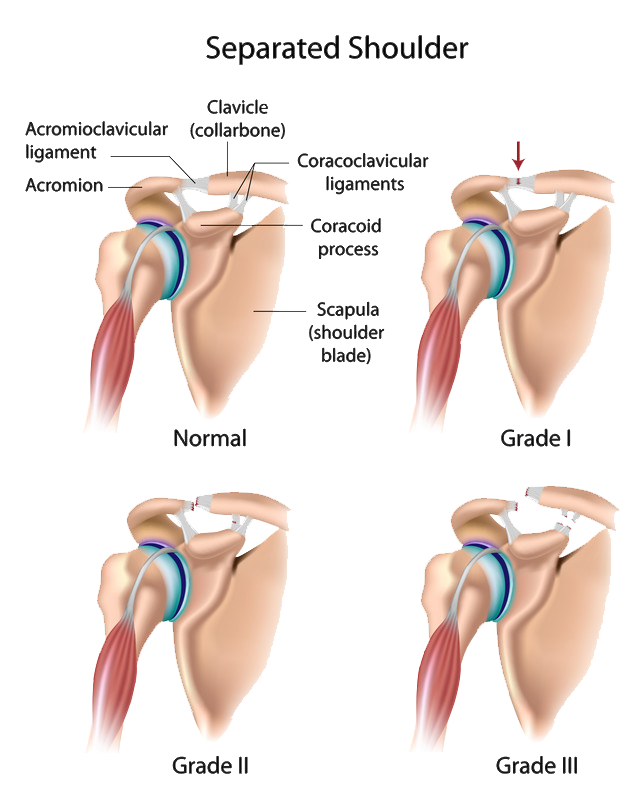
A-C Joint Stabilization/Reconstruction
The acromioclavicular joint (AC joint) is located at the top of the shoulder. It works as the junction between the acromion and the clavicle. A common injury to the joint is and acromioclavicular joint separation. When this happens, the collar bone separates from the scapula, usually due to a fall or direct blow.
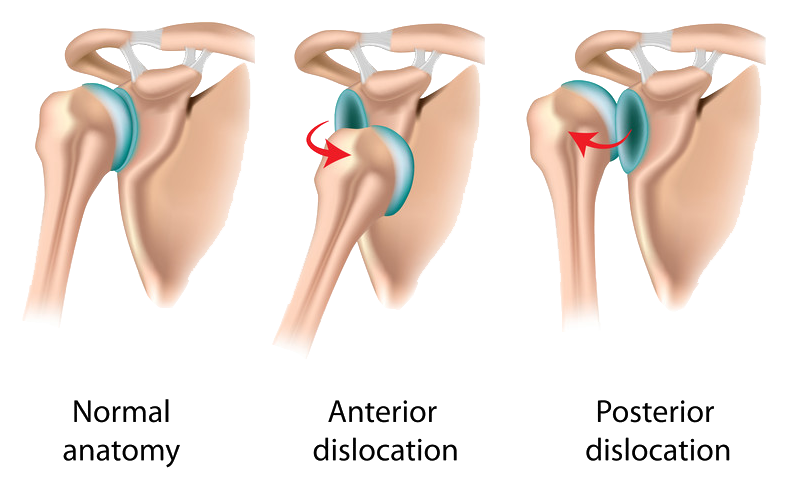
Causes of Shoulder Instability
A dislocation occurs when the head of the humerus is forced out of the glenoid. If it is only partially forced out, it is known as subluxation. If the shoulder is repeatedly experiencing dislocation or subluxation, it is said to be suffering from instability. A weakened capsule and ligaments of the shoulder joint cause the instability, allowing the ball to fall out of the socket. The process is very painful, and with the shoulder feeling so unstable, everyday activities may be severely modified for fear of reoccurrence.
Injury or trauma is what usually causes dislocations and some subluxations. Trauma is a strong impact to the region; sometimes it can even occur from using the hand to stop a fall, which jolts the shoulder region. Unfortunately, some patients simply have unstable shoulders that sublux or dislocate on their own without trauma.
Instability can cause further problems with injury to the rotator cuff. Instability can also cause pain, because the rotator cuff is constantly trying to stabilize the loose shoulder. Doctors call this instability tendonitis (or secondary impingement). Internal impingement occurs when instability in the shoulder causes it to rotate too much. The rotator cuff is forced to bump up against the glenoid, and subsequently it starts to tear the labrum and the posterior superior rotator cuff.
Dislocations and subluxations can cause tears of the labrum, ligaments, or capsule in addition to tears in the rotator cuff. They may also cause fractures of the shoulder joint.
Shoulder Stabilization/Reconstruction Surgery
The aim of surgery is to help make the shoulder stable again by reducing the size of the stretched area, and attaching the labrum back onto the bone. The procedure repairs the shoulder joint and tighten any loosening/stretching that has occurred. Your doctor will conduct a thorough examination to determine if there is any damage to muscles or nerves, and how much damage needs repairing.
Surgery is generally performed through arthroscopy. After anesthetic is administered, your doctor will inspect the shoulder joint. Tendon tears, cartilage tears and/or joint inflammation may be encountered.
To address the labral tear, the surface of surrounding bone is roughened so that it has a sticky texture on the surface. Holes are then drilled in the bone and anchors inserted. Sutures act as ropes for the anchors to be attached to the torn tissue.
Following the procedure, the shoulder will be much more stable and less prone to further injury.
Stryker InSpace Balloon
The InSpace™ implant is a first-of-its-kind biodegradable subacromial balloon spacer designed for the arthroscopic treatment of massive irreparable rotator cuff tears (MIRCTs).
The InSpace balloon provides a shorter, less invasive option for patients with rotator cuff injuries and facilitates continuous, clinically substantial improvements in the function and symptoms of the patient’s shoulder.

I have had three surgeries performed by Dr. Sima over this past year. The “results” of all three of the surgeries were far in excess of my expectations. Often times many people experience “excellence” within the Medical world, but rarely does a surgeon come along that is in that elite category that is above “excellent”. Dr. Sima is in that category.
-Peter Clyde
Non-Surgical Shoulder Procedures
Many surgery alternatives are available for those whose injuries and conditions can still be treated without requiring surgical intervention. Please explore these options below and contact our office to book your appointment and discuss your options.
What is Mesenchymal Progenitor Cell (MPC) Therapy?
Your body consists of billions of cells that degenerate and regenerate in a daily cycle. As older cells die off, new cells are created from the stem cells. The cells form organs of the body such as skin, muscles, ligaments, joints, bone, tendons and the brain. Unfortunately, if tissue is damaged, the degenerative process dominates the cycle and the organs will become less functional, and pain will often result. The stem cells used for MSC are found in your own bone marrow and are known as mesenchymal cells.
How Does it Work?
- Stem cells are obtained from the patient’s body, generally from within the bone marrow of the hip area.
- The procedure takes place in our clinic, under ultrasound or x-ray guidance
- You will lie face down and the doctor will thoroughly clean the area. Next, a needle penetrates the bone and will remove blood from within the marrow, which contains the stem cells.
- After the procedure, the stem cell rich blood is taken to the laboratory where it is concentrated, cells that are not required are removed, and the remaining stem cells purified.
- The stem cells are injected precisely by hand into the injured tissues in other areas of the body using MSK Ultrasound for guidance. Through imaging devices, your doctor can ensure the cells are injected precisely at the site of need.
Which Conditions Benefit from MSC Therapy?
Degenerative conditions such as osteoarthritis and joint injuries respond well to MSC therapy. Contact our office to find out whether you are a candidate for this advanced procedure
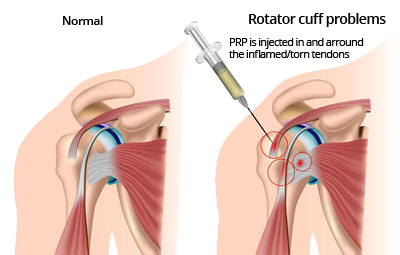
Platelet-rich Plasma (PRP) Treatment
Platelet-rich Plasma Treatment, also known as PRP, is a popular treatment method for a variety of shoulder problems, often used by Athletes due to its lack of negative side effects and the fact there is little recovery time needed after the procedure.
What is Platelet-Rich Plasma (PRP)
Though our blood seems to be all liquid (which is called plasma), it contains very small solid parts such as red cells, white cells, and platelets. Platelets play an important role in helping blood to clot, and platelets also contain growth factors that help the body heal itself.
How Does PRP Work?
First, blood is removed from the patient. Platelets are separated and removed from the other blood components through a process known as centrifugation. The increased concentration of growth factors in PRP speed up the body’s healing process. PRP is gently injected into the site of the injury. PRP can also be used to aid in healing after surgery for some injuries.
What Conditions Benefit from PRP?
A number of conditions may benefit from PRP treatment, but it is important to visit our office to determine whether your unique condition will be suitable for this treatment.
Some common problems that have been successfully treated by PRP include:
- Chronic and acute tendon injuries
- Acute Ligament and Muscle Injuries
- Arthritis