Hip Injuries
Hip injuries are painful and inconvenient. It is important to quickly identify what your injury is and what your treatment options may be. Below you will find symptoms, treatment options, and other information about various hip injuries. Please contact us to request an orthopaedic evaluation.
Arthritis of the Hip
Whether you have just begun exploring treatment options or have already decided to undergo hip replacement surgery, this information will help you understand the benefits and limitations of total hip replacement. This article describes how a normal hip works, the causes of hip pain, what to expect from hip replacement surgery, and what exercises and activities will help restore your mobility and strength, and enable you to return to everyday activities.
If your hip has been damaged by arthritis, a fracture, or other conditions, common activities such as walking or getting in and out of a chair may be painful and difficult. Your hip may be stiff, and it may be hard to put on your shoes and socks. You may even feel uncomfortable while resting.
If medications, changes in your everyday activities, and the use of walking supports do not adequately help your symptoms, you may consider hip replacement surgery. Hip replacement surgery is a safe and effective procedure that can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities.
First performed in 1960, hip replacement surgery is one of the most successful operations in all of medicine. Since 1960, improvements in joint replacement surgical techniques and technology have greatly increased the effectiveness of total hip replacement. According to the Agency for Healthcare Research and Quality, more than 300,000 total hip replacements are performed each year in the United States.
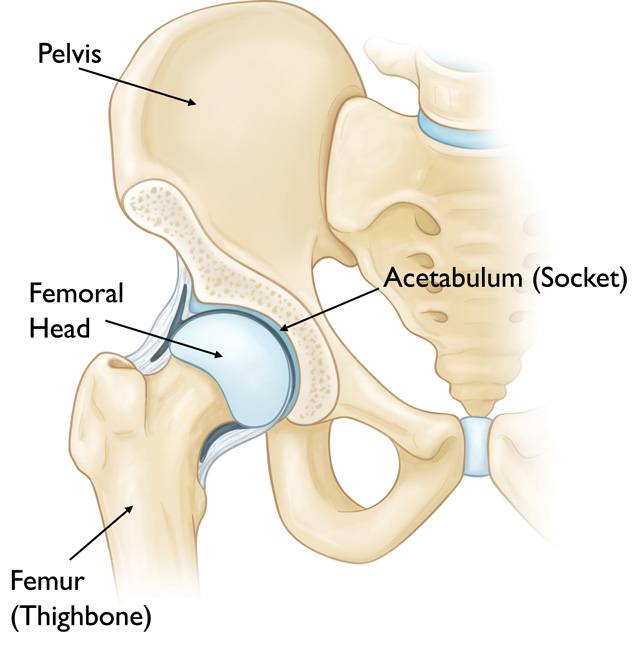
The hip is one of the body’s largest joints. It is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
The bone surfaces of the ball and socket are covered with articular cartilage, a smooth tissue that cushions the ends of the bones and enables them to move easily.
A thin tissue called synovial membrane surrounds the hip joint. In a healthy hip, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost all friction during hip movement.
Bands of tissue called ligaments (the hip capsule) connect the ball to the socket and provide stability to the joint.
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and traumatic arthritis are the most common forms of this disease.
- Osteoarthritis. This is an age-related “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older and often in individuals with a family history of arthritis. The cartilage cushioning the bones of the hip wears away. The bones then rub against each other, causing hip pain and stiffness. Osteoarthritis may also be caused or accelerated by subtle irregularities in how the hip developed in childhood.
- Rheumatoid arthritis. This is an autoimmune disease in which the synovial membrane becomes inflamed and thickened. This chronic inflammation can damage the cartilage, leading to pain and stiffness. Rheumatoid arthritis is the most common type of a group of disorders termed “inflammatory arthritis.”
- Post-traumatic arthritis. This can follow a serious hip injury or fracture. The cartilage may become damaged and lead to hip pain and stiffness over time.
- Avascular necrosis. An injury to the hip, such as a dislocation or fracture, may limit the blood supply to the femoral head. This is called avascular necrosis (also commonly referred to as “osteonecrosis”). The lack of blood may cause the surface of the bone to collapse, and arthritis will result. Some diseases can also cause avascular necrosis.
- Childhood hip disease. Some infants and children have hip problems. Even though the problems are successfully treated during childhood, they may still cause arthritis later on in life. This happens because the hip may not grow normally, and the joint surfaces are affected.

Symptoms
- A dull, aching pain in the groin, outer thigh, knee, or buttocks
- Pain that is worse in the morning or after sitting, but that lessens with activity
- Increase pain and stiffness with vigorous activity
- Pain in the joint severe enough to cause a limp or make walking difficult
Surgical Options
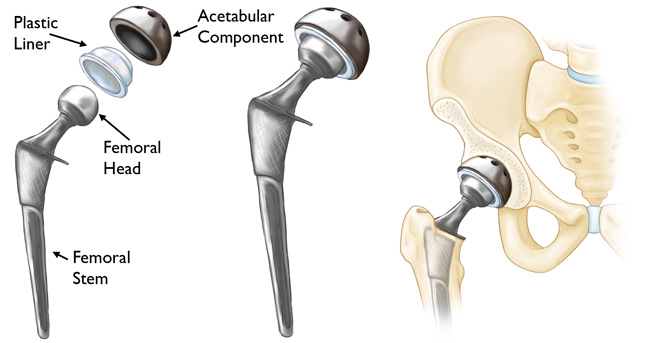
In a total hip replacement (also called total hip arthroplasty), the damaged bone and cartilage is removed and replaced with prosthetic components.
- The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur. The femoral stem may be either cemented or “press fit” into the bone.
- A metal or ceramic ball is placed on the upper part of the stem. This ball replaces the damaged femoral head that was removed.
- The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket. Screws or cement are sometimes used to hold the socket in place.
- A plastic, ceramic, or metal spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.
Non-Surgical Options
- There are many emerging surgery alternatives, such as PRP injections and stem cell treatments for healing a variety of hip conditions.
- Non-steroidal anti-inflammatory drugs, such as ibuprofen to help reduce pain and inflammation
- Corticosteroids
- Disease-modifying antirheumatic drugs (DMARDs)
- Physical therapy
- Regular, moderate exercise may decrease stiffness and improve endurance
- Assistive devices, such as a cane, walker, long-handled shoehorn, or reacher may make it easier to perform daily living tasks
Femoroacetabular Impingement Syndrome (FAI)
Femoroacetabular impingement (FAI) is a condition in which extra bone grows along one or both of the bones that form the hip joint — giving the bones an irregular shape. Because they do not fit together perfectly, the bones rub against each other during movement. Over time this friction can damage the joint, causing pain and limiting activity.
Anatomy
The hip is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
A slippery tissue called articular cartilage covers the surface of the ball and the socket. It creates a smooth, low friction surface that helps the bones glide easily across each other during movement.
The acetabulum is ringed by strong fibrocartilage called the labrum. The labrum forms a gasket around the socket, creating a tight seal and helping to provide stability to the joint.

Description
In FAI, bone overgrowth — called bone spurs — develop around the femoral head and/or along the acetabulum. This extra bone causes abnormal contact between the hip bones, and prevents them from moving smoothly during activity. Over time, this can result in tears of the labrum and breakdown of articular cartilage (osteoarthritis).
Types of FAI
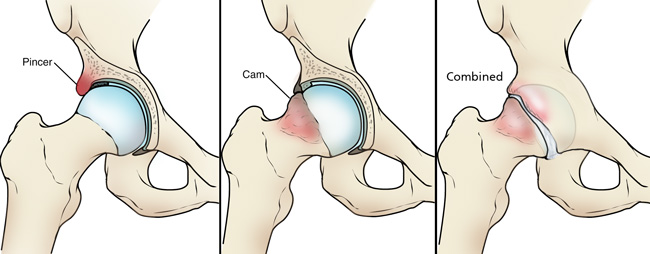
There are three types of FAI: pincer, cam, and combined impingement.
- Pincer. This type of impingement occurs because extra bone extends out over the normal rim of the acetabulum. The labrum can be crushed under the prominent rim of the acetabulum.
- Cam. In cam impingement the femoral head is not round and cannot rotate smoothly inside the acetabulum. A bump forms on the edge of the femoral head that grinds the cartilage inside the acetabulum.
- Combined. Combined impingement just means that both the pincer and cam types are present.
Cause
FAI occurs because the hip bones do not form normally during the childhood growing years. It is the deformity of a cam bone spur, pincer bone spur, or both, that leads to joint damage and pain. When the hip bones are shaped abnormally, there is little that can be done to prevent FAI.
It is not known how many people have FAI. Some people may live long, active lives with FAI and never have problems. When symptoms develop, however, it usually indicates that there is damage to the cartilage or labrum and the disease is likely to progress.
Because athletic people may work the hip joint more vigorously, they may begin to experience pain earlier than those who are less active. However, exercise does not cause FAI.
Symptoms
The most common symptoms of FAI include:
- Pain
- Stiffness
- Limping
Pain often occurs in the groin area, although it may occur toward the outside of the hip. Turning, twisting, and squatting may cause a sharp, stabbing pain. Sometimes, the pain is just a dull ache.
Surgical Options
If tests show joint damage caused by FAI and your pain is not relieved by nonsurgical treatment, your doctor may recommend surgery.
Arthroscopy
Many FAI problems can be treated with arthroscopic surgery. Arthroscopic procedures are done with small incisions and thin instruments. The surgeon uses a small camera, called an arthroscope, to view inside the hip.
During arthroscopy, your doctor can repair or clean out any damage to the labrum and articular cartilage. He or she can correct the FAI by trimming the bony rim of the acetabulum and also shaving down the bump on the femoral head.
Non-Surgical Options
Activity changes. Your doctor may first recommend simply changing your daily routine and avoiding activities that cause symptoms.
Non-steroidal anti-inflammatory medications. Drugs like ibuprofen can be provided in a prescription-strength form to help reduce pain and inflammation.
Physical therapy. Specific exercises can improve the range of motion in your hip and strengthen the muscles that support the joint. This can relieve some stress on the injured labrum or cartilage.
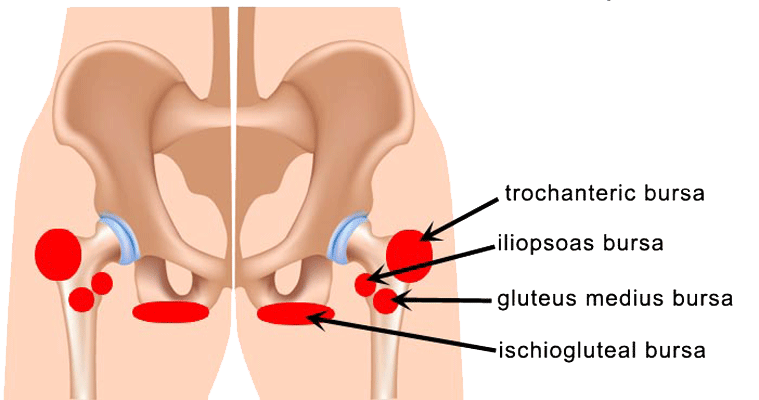
Bursitis
Bursae are small, jelly like sacs are located throughout the body – especially in joints where a lot of movement occurs, like the hip. Their purpose is to reduce friction and act as cushions during joint movement. Bursitis is inflammation of the bursa.
Bursitis related to the hip may be experienced in two places. The first is on the outside of the hip joint, affecting the greater trochanter of the femur (just next to the femoral head), which is called trochanteric bursitis. The second is called hip bursitis, or more specifically, iliopsoas bursitis, and is felt in the groin area.
Symptoms
Inflammation of a bursa is caused by repetitive-use injuries, prolonged pressure, lumbar spine diseases, rheumatoid arthritis, or sometimes infection. It can affect anyone at any age, but is most common in women and the middle-aged. The main symptom is aching pain in the outer hip. The pain worsens with movement or pressure and may travel down the outside of the thigh toward the knee. Pain caused by pressure at night can make sleeping very difficult.
Surgical Options
Surgery to remove the damaged bursa may be an option in severe cases.
Non-Surgical Options
- Initial treatment of bursitis involves resting, immobilizing the area, and non-steroidal anti-inflammatory medications to reduce inflammation and relieve pain. This regimen is often effective.
- Exercise and physical therapy – especially for the hip and lower back – can be helpful to strengthen the surrounding muscles and help prevent further episodes.
- If these measures don’t relieve the pain, a doctor may recommend an injection of corticosteroids around the bursa, which usually brings rapid pain relief.
Labral Tear
The labrum is a ring of cartilage that follows the outside rim of the hip joint, and helps to cushion the joint. It also acts like a rubber seal helping to hold the back part of the femur into the hip socket. A hip labral tear involves damage to this cartilage.
Symptoms
While many labral hip tears do not produce symptoms, patients may experience the following:
- A limited range of motion at the hip joint, with or without accompanying stiffness
- Pain in the hip or groin area
- A sensation of locking or clicking in the hip joint
Surgical Options
- If nonsurgical treatments do not produce desired results, then arthroscopic labral repair surgery may be an option. In this procedure, a fiber-optic camera and surgical tools are inserted into the skin via a small incision. The surgeon may choose to cut out and remove a torn piece of labrum, or may decide to repair the tissue by sewing it back together
Non-Surgical Options
- Avoid activities that worsen symptoms
- Non-steroidal anti-inflammatory drugs, such as ibuprofen to help reduce pain and inflammation
- An injection of corticosteroids into the joint can temporarily control pain
Hamstring/Muscle Injuries
The hamstring muscles run down the back of the thigh and are heavily involved in day to day activities such as running, jumping, standing, and general posture. The hamstrings are made up of three main muscles: the semitendinosus, the semimembranosus, and the biceps femoris. A pulled hamstring or strain is an injury to one of these muscles. These injuries are very common, and occur most frequently in athletes who perform sprinting, such as track, soccer, and basketball. Most hamstring injuries respond well to simple, nonsurgical treatments.
Symptoms
- Hamstring injuries during sprinting or intense activity will be accompanied by a sudden, sharp pain in the back of the thigh
- Patients may also experience swelling during the first few hours after injury
- Bruising or discoloration on the back of the leg below the knees over the first few days
- Weakness in the hamstrings that can persist for weeks
Surgical Options
Surgery is usually performed when there has been a full avulsion, which is when the tendon pulls away from the bone. Surgery may also be needed to repair a complete tear of the muscle tissue itself.
- To repair an avulsion, the surgeon will pull the muscle and tendon back into shape, and use large stitches and staples to anchor the tendon back to the bone
- A complete tear to the muscle is sewn back together using stitches
- Rehabilitation accompanies any surgery, and may last for up to 6 months, however most people will recover full function of their hamstrings
To prevent any further tears or avulsions, be sure to follow your doctor’s advice.
Non-Surgical Options
- The RICE protocol
- Rest – take a break from the activity that caused the strain, including using crutches to avoid putting weight on the leg
- Ice – use cold packs several times a day for up to 20 minutes at a time, remembering not to apply ice directly to the skin
- Compression – wear an elastic compression bandage to prevent additional swelling and blood loss
- Elevation – recline and put the leg up to reduce swelling
- Immobilization is used to keep the leg in a neutral position so that it will heal. This is achieved by using a knee splint, often for a brief time only
- Physical therapy can begin once the initial swelling has gone down, and will use specific exercises to restore strength and affected range of motion
Dear Dr. Sima,
I am writing to express my appreciation to you for providing the surgical skills needed for my recent hip replacement surgery. I am grateful for the commitment you’ve made to continually learn and use innovative techniques which benefit your patient’s successful surgery and recovery.
-Rick Runnels