Hand & Wrist Surgery
Surgery and Surgery Alternatives
Surgical Hand & Wrist Procedures
Hand & wrist surgery may be the best option for your hand or wrist injury, but there are surgery alternatives as well. We offer the latest in medical advancement to ensure that we find the best treatment for your injury or condition. Review hand and wrist surgery and surgery alternative options, success rates, recovery times, and more below.
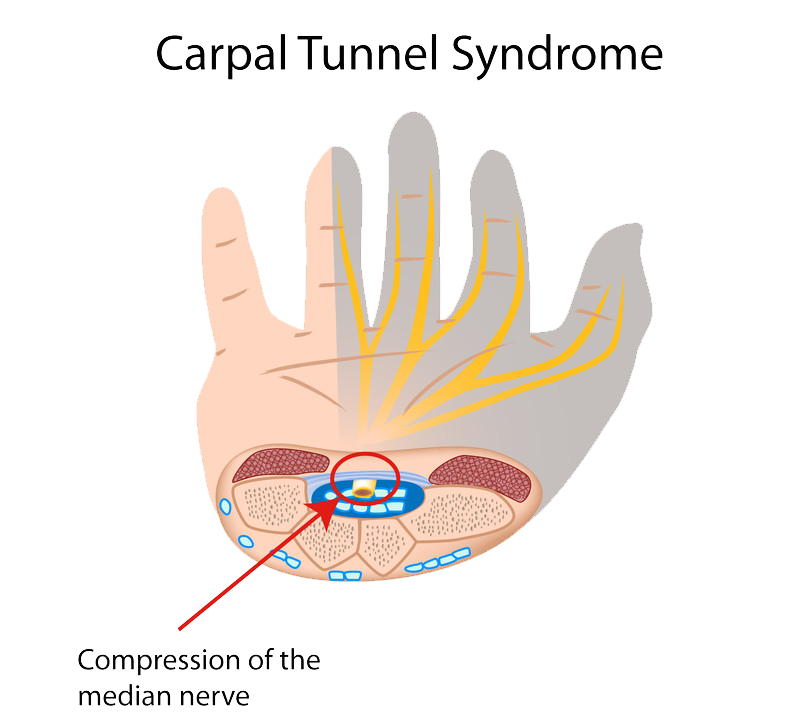
Carpal Tunnel Release Surgery
The surgical procedure used to treat patients with carpal tunnel syndrome is called carpal tunnel release. This procedure can be performed as open carpal tunnel release or endoscopic carpal tunnel release. Both aim to relieve pressure on the median nerve, which is achieved by cutting the ligament that forms the roof of the carpal tunnel.
Carpal tunnel surgery is usually performed on an outpatient basis under local or general anesthetic.
Open Carpal Tunnel Release Surgery
In open surgery, a small cut is made into the palm of the hand so the surgeon can view inside of the hand and wrist. The transverse carpal ligament (the roof of the carpal tunnel) is cut in order to create more space in the carpal tunnel and to decrease pressure on the median nerve.
The ligaments will gradually grow back together, but there will still be more room in the carpal tunnel than before the surgery, and therefore less pressure on the nerve.
Endoscopic Carpal Tunnel Release
Endoscopic carpal release surgery makes use of an endoscope (small camera) to see inside the hand and wrist. The camera is inserted through two small skin incisions. Guided by the camera, the transverse carpal ligament is divided in a similar way to open carpal tunnel surgery.
Dr. Sima is a specialist in carpal tunnel release surgery and will discuss which surgical technique is best for you.
Thumb CMC Arthroplasty
Thumb CMC arthroplasty is used to treat osteoarthritis in the thumb. This form of arthritis affects the carpometacarpal (CMC) joint, located at the base of the thumb. The CMC joint is what helps with movement in the thumb (up/down/across) and enables us to pinch. The two bones found in the joint are covered with cartilage that helps absorb shock and allows smooth movements.
Osteoarthritis causes the cartilage to wear down and leads to chronic pain and inflammation, making treatment necessary.
Thumb CMC Arthroplasty Surgical Procedure
The purpose of Thumb CMC arthroplasty is to remove the small wrist bone (trapezium) that is part of the CMC joint and to replace it with a wrist flexor tendon.
- Under general anesthesia, a small 1.5 inch incision is made above the CMC joint, and the trapezium wrist bone is removed.
- Another incision is made in the forearm and is used to access the wrist flexor tendon. This tendon is attached to the base of the metacarpal bone in the base of the thumb using an anchor and the remaining tendon is pushed into the hole left by the removal of the trapezium. This protects the remaining bones by providing cushioning.
- Dissolvable sutures close the incision and a cast is used to immobilize the operation region.
De Quervain’s Tendinosis
De Quervain’s tendinosis is a condition that occurs at the base of the thumb, caused by irritated and constricted tendons. The term tendinosis refers to swelling in the tendons. The result is pain and tenderness along the thumb-side of the wrist, especially when the patient tries to form a fist, turn the wrist, or hold onto something.
Symptoms of De Quervain’s Tendinosis
De Quervain’s tendinosis is usually caused by overuse, and is often diagnosed in pregnant woman or those with rheumatoid arthritis. Middle aged woman are most often affected by this condition. Signs you may have De Quervain’s tendonitis include:
- Pain on the thumb-side of the wrist that comes on gradually or suddenly. The pain is usually felt in the wrist and radiates up the arm. When the hand and thumb are use the pain is often worse.
- Swelling may be visible on the thumb-side of the wrist. At times, a cyst may form in the region.
- You may feel a “catching” or “snapping” sensation when you move your thumb.
A specialist will normally perform a Finkelstein test to determine whether you have De Quervain’s tendinosis. The test involves placing your thumb and hand in different positions. If you have de Quervain’s tendinosis, this test can be quite painful.
Nonsurgical Treatment
Treatment of de Quervain’s tendinosis aims to relieve the pain caused by irritation and swelling.
- Splints
The use of splints may help rest the thumb and wrist.
- Anti-inflammatory medication (NSAIDs)
Anti-inflammatory medicines (such as Ibuprofen) may help reduce swelling and relieve pain.
- Modifying or eliminating activities that cause pain and swelling
Symptoms may cease when these activities are avoided.
- Corticosteroid Injections
Injection of corticosteroids can be administered straight into the tendon sheath and may help reduce swelling and pain.
Surgical Treatment
If the tendonitis is too severe, surgery may be recommended. Surgery aims to open up the thumb compartment, making more space for the irritated tendons.
- A relatively painless procedure is performed on an outpatient basis where a small incision is made and the tendons are released in order for them to heal.
- In some patients, simply releasing tendons can cause them to sublux, making them “snap.” Your surgeon may decide to perform a further procedure that lengthens the fascia in order to prevent subluxation.
- Following surgery, a splint is worn for a few days to provide extra support and prevent movement during the healing process.
Following the procedure, the patient should have normal use of the hand again.
Distal Radius Fractures (Broken Wrist)
The forearm consists of two bones, and the larger of the two is the radius. The end of the radius that meets the wrist is known as the distal end, making a distal radius fracture a broken bone at the wrist-end of the radius bone. The most commonly broken bone in the arm is the radius bone.
There are many ways the bone can break, but the break is usually about 1 inch from the base of the bone. Different fracture types include colles (where the bone fragment tilts upward), intra-articular (where the fracture extends into the wrist joint), extra-articular (the fracture doesn’t extend into the joint), comminuted (the bone is broken in more than two pieces) and open fracture (where the fractured bone breaks through the skin).
The ulna bone in the forearm may also become fractured. This is known as distal ulnar fracture.

Distal Radius Fracture Treatment
In order to determine the extent of the injury and the right treatment, a thorough investigation including X-rays will be undertaken.
Nonsurgical Treatment
- A plaster cast may be used to hold the bone in the correct position for healing.
- Re-alignment of the bone may be necessary if it is out of place and having an affect on function. This is known as reduction. This procedure may need to be done through incisions, or without having to open the skin in a process known as a closed reduction.
- A splint is needed for a few days after reduction due to swelling. Afterwards, a cast is necessary for up to 6 weeks.
- Physical therapy is often required after the cast is removed to help improve motion and regain function of the wrist.
Surgical Treatment
When the bone cannot be corrected with a cast it can cause long-term problems with the function of the arm. In this case, surgery is often necessary.
- A metal plate and screws/pins may be used to hold the broken fragments in position while they heal. This is done under general anesthetic.
- In the case of open fractures, urgent surgery following the injury is required (within 8 hours). Exposed soft tissue and bone are at great risk of infection, so antibiotics are often administered as a precaution. Your surgeon may use external or internal fixation methods to hold the bones in place.
Whether surgical or non surgical methods are used to help your fracture heal, there will generally be moderate pain associated with your injury. Some techniques to help ease the pain include:
- Ice
- Elevation (raising your arm above the level of your heart)
- Pain medication (a combination of ibuprofen and acetaminophen seem to be the best combination for pain relief). In severe cases, opioids may be prescribed. However, these must be used with caution under strict guidance from your doctor.
Recovery time can vary depending on the severity of the fracture and treatment method. In general, light activities can resume after 1-2 months, vigorous activities 3 – 6 months later, and full function around 12 months after treatment.
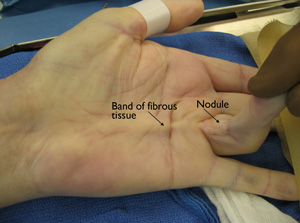
Dupuytren’s Contracture
Dupuytren’s contracture is a thickening of the fibrous tissue layer underneath the skin of the palm and fingers. Although painless, the thickening and tightening (contracture) of this fibrous tissue can cause the fingers to curl (flex).
Dupuytren’s contracture is more common in men than in women.
Cause
The cause of Dupuytren’s contracture is not known. It is not caused by an injury or heavy hand use.

There are factors that put people at greater risk for developing Dupuytren’s contracture.
- It is most common in people of Northern European (English, Irish, Scottish, French, Dutch) or Scandinavian (Swedish, Norwegian, Finnish) ancestry.
- It often runs in families (hereditary).
- It may be associated with drinking alcohol.
- It is associated with certain medical conditions, such as diabetes and seizures.
- It increases in frequency with age.
Symptoms
Dupuytren’s contracture symptoms usually occur very gradually.
Nodules. One or more small, tender lumps (nodules) form in the palm. Over time, the tenderness usually goes away.
Bands of tissue. The nodules may thicken and contract, forming tough bands of tissue under the skin.
Curled fingers. One or more fingers bend (flex) toward the palm. The ring and little fingers are most commonly affected, but any or all fingers can be involved. As the bend in the finger increases, it may be hard to straighten your finger. Grasping large objects and putting your hand in a pocket becomes difficult.
Doctor Examination
Your doctor will examine your hand and test the feeling in your thumb and fingers. Your grip and pinch strength may also be tested.
During the examination, your doctor will record the locations of nodules and bands on your palm. Using a special device, he or she will measure the amount of contracture in your fingers. Your doctor may also measure the range of motion in your fingers to determine whether there is limitation in your flexion.
Your doctor will refer back to these measurements throughout your treatment to determine whether the disease is progressing.
Treatment
There is no way to stop or cure Dupuytren’s contracture. However, it is not dangerous. Dupuytren’s contracture usually progresses very slowly and may not become troublesome for years. It may never progress beyond lumps in the palm.
If the condition progresses, nonsurgical treatment may help to slow the disease.
Nonsurgical Treatment
Steroid injection. If a lump is painful, an injection of corticosteroid – a powerful anti-inflammatory medication – may help relieve the pain. In some cases, it may prevent the progression of contracture. Several injections may be needed for a lasting effect.
Splints. Splinting does not prevent increased bend in the finger. Forceful stretching of the contracted finger will not help either, and may speed the progression of contracture.
Surgical Treatment
Surgery is recommended when your doctor has confirmed through measurements over time that the disease is progressing. Some patients turn to surgical treatment when hand function is limited; they have trouble grasping objects or putting their hands in their pockets.
Surgical procedure. Surgery for Dupuytren’s contracture divides or removes the thickened bands to help restore finger motion. Sometimes the wound is left open and allowed to heal gradually. Skin grafting may be needed.
Complications. Although rare, risks of surgery include injury to nerves and blood vessels, and infection. Permanent stiffness of the fingers may occur, although this is also rare.
Recovery. Some swelling and soreness are expected after surgery, but severe problems are rare.
After surgery, elevating your hand above your heart and gently moving your fingers help to relieve pain, swelling, and stiffness.
Physical therapy may be helpful during recovery after surgery. Specific exercises can help strengthen your hands and help you move your fingers. Most people will be able to move their fingers better after surgery.
Recurrence. Approximately 20% of patients experience some degree of recurrence. This may require further surgery.
Trigger Finger Surgery
Trigger finger is a condition involving a tendon in the finger or thumb that forces your finger/thumb to lock up before it can pop out straight again.
Surgical Treatment
If your finger is stuck in a bent position, your doctor may recommend surgery to prevent permanent stiffness. Surgical procedures for trigger finger are usually performed on an outpatient basis using local anesthetic.
Procedure
First, a small incision is made in the palm of the hand. The sheath of the affected tendon is then cut. Over time as the sheath heals it will become looser, making it easier for the tendon to move. Following the surgery, it is normal to have some soreness in the palm. Stiffness and swelling will gradually decrease following the procedure and some exercises may be recommended to aid with healing.

I have had three surgeries performed by Dr. Sima over this past year. The “results” of all three of the surgeries were far in excess of my expectations. Often times many people experience “excellence” within the Medical world, but rarely does a surgeon come along that is in that elite category that is above “excellent”. Dr. Sima is in that category.
-Peter Clyde