Ankle & Foot Injuries
Foot & ankle injuries are painful and inconvenient.It is important to quickly identify what your injury is and what your treatment options may be. Below you will find symptoms, treatment options, and other information about various foot & ankle injuries. Please contact us to request an orthopaedic evaluation.
Ankle Tendonitis
Foot and ankle tendonitis is a common problem that occurs when there is inflammation or irritation of the tendons. There are a number of tendons in the foot that can result in conditions such as achilles tendonitis and extensor tendonitis. The main cause of foot and ankle tendonitis is usually one of the following:
- Overuse – when the tendon has to work to hard or is being overstretched repeatedly
- Injury – repetitive friction on the tendon (i.e. shoe rubbing) or following an ankle injury
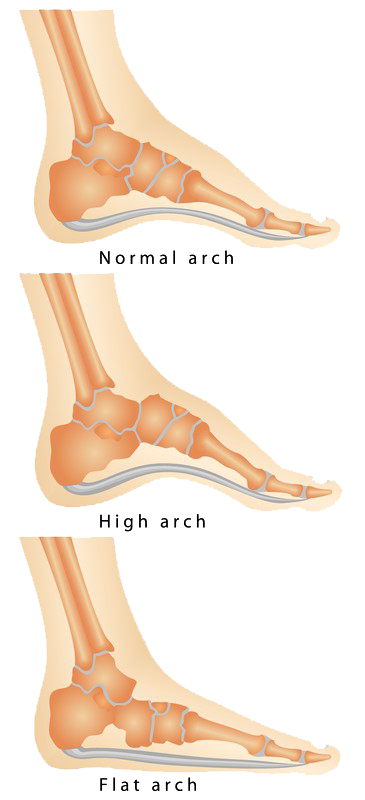
- Abnormal foot structure – flat foot or high arches can put too much stress on the tendons
- Medical conditions – conditions such as gout and arthritis that involve inflammation can cause foot tendonitis
Symptoms
- Swelling – a small tender lump may form over the tendon
- Pain – usually a sharp or burning pain
- Stiffness
Surgical Options
When non-surgical methods of treatment do not improve symptoms, a surgical procedure that involves repairing or removing inflamed tissue and eliminating any bone spurs that irritate the tendon may be necessary. It is important to have your condition evaluated to determine the best treatment and prevent further injury.
Non-Surgical Options
- Modifying or avoiding activities that worsen symptoms
- Applying ice to the ankle several times a day
- Using soft cushioning heal inserts in your shoes
- Reducing weight
- Gentle stretching exercises
- Nonsteroidal anti-inflammatory drugs to reduce pain and swelling
- Wearing a brace or special boot to help stabilize your joint
- Extracorporeal shockwave therapy may be recommended if symptoms don’t reduce after 3 months
Ankle & Foot Arthritis
Arthritis is inflammation of one or more joints. Pain and stiffness result and many everyday activities can become difficult. Given the many small joints in the ankle and foot, arthritis is quite common.
The most common types of arthritis affecting the foot and ankle are:
- Osteoarthritis – common after middle age, osteoarthritis is a degenerative condition caused by long term use or overuse of the joints. Osteoarthritis develops slowly and over time pain and stiffness increase if left untreated.
- Rheumatoid Arthritis – this is an autoimmune disease that affects a number of joints in the body, usually starting in the foot and ankle. It is symmetrical, meaning that it usually affects the same joint on both sides of the body.
- Post-Traumatic Arthritis – this form of arthritis can form after injury to the foot or ankle if damage to the joint surface occurs.

Symptoms
The symptoms of arthritis vary depending on which joint is affected. Normally, any pain associated with the condition develops gradually over time. Common symptoms include:
- Pain with movement
- Pain that worsens with activity
- Tenderness in the joint area
- Swelling, warmth, and redness in the joint area
- Increased pain and swelling in the morning, or after sitting or resting
- Difficult movement
Surgical Options
If the pain or decreased movement caused by arthritis is not helped by non surgical treatments, a specialist may recommend surgery. The type of surgery will depend on which joint is affected and the type of arthritis observed. Common forms of surgery include:
Arthroscopic debridement. Debridement is a procedure that aims to remove loose cartilage, inflamed synovial tissue, and bone spurs from around the joint, essentially “cleaning” out the joint area.
Arthrodesis. Arthrodesis fuses the bones of the joint together to make one bone and significantly reduces motion in the joint to help reduce pain.
Total ankle replacement (arthroplasty). In total ankle replacement, the damaged cartilage and bone are removed, and synthetic joint surfaces (normally metal or plastic) are installed to help restore function to the joint.
Non-Surgical Options
Your doctor will initially recommend non-surgical treatment options. These may include:
Lifestyle modifications. Changes in daily activities to help slow the progression of the disease. These modifications may include:
- Reducing activities that make the symptoms worse
- Changing from high-impact activities to lower impact activities to help reduce stress on the foot and ankle.
- Weight reduction to reduce stress on the joints.
Physical therapy. Specific exercises designed to help increase range of motion and flexibility, as well as help strengthen the muscles in the foot and ankle.
Assistive Devices. Braces or orthotics can help minimize pressure and pain, and a cane can help with stability.
Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can help reduce swelling and relieve pain. In severe cases, cortisone may be injected into an arthritic joint.
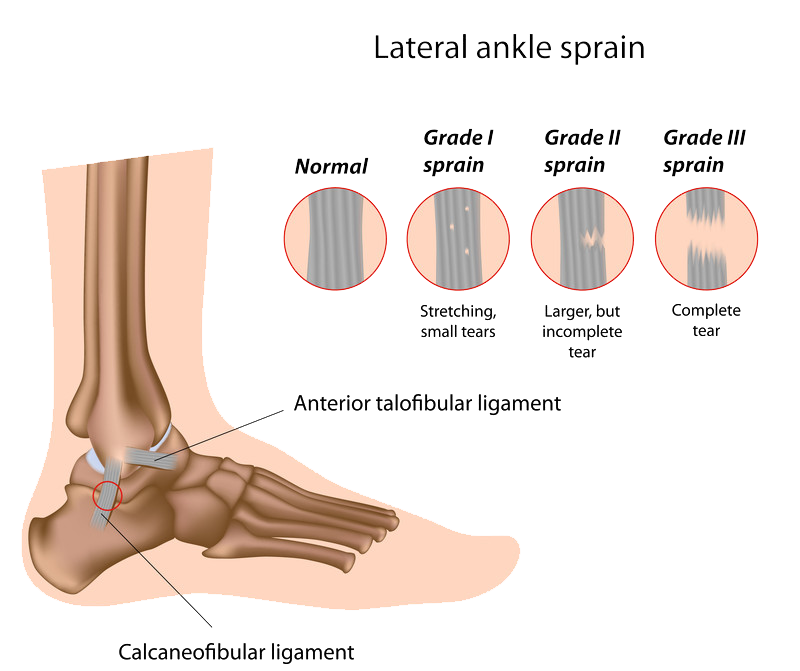
Ankle & Foot Fractures
Fractures are normally caused by heavy impact to the foot, accidents, rolling or twisting your ankle, or overuse from particular activities.
Symptoms
The most common symptoms of a fracture include:
- Bruising
- Severe pain
- Pain when walking and weight bearing
- Tenderness
- Inability to put any weight on the injured foot
- Deformity in the foot
Surgical Options
When the fracture is severe, surgery may be necessary. Depending on the fracture, the bone fragments may be fixed using screws, a plate, and/or wiring.
Non-Surgical Options
Treatment for fractures varies greatly depending on the bone that was fractured and the severity. Nonsurgical treatment options may include:
- First aid
- Applying ice to help reduce swelling.
- Elevating the foot
- Limiting weight bearing
- Lightly wrapping the foot with a compression dressing
- Taping/strapping
- Manipulating the bone back into place
- Elevation
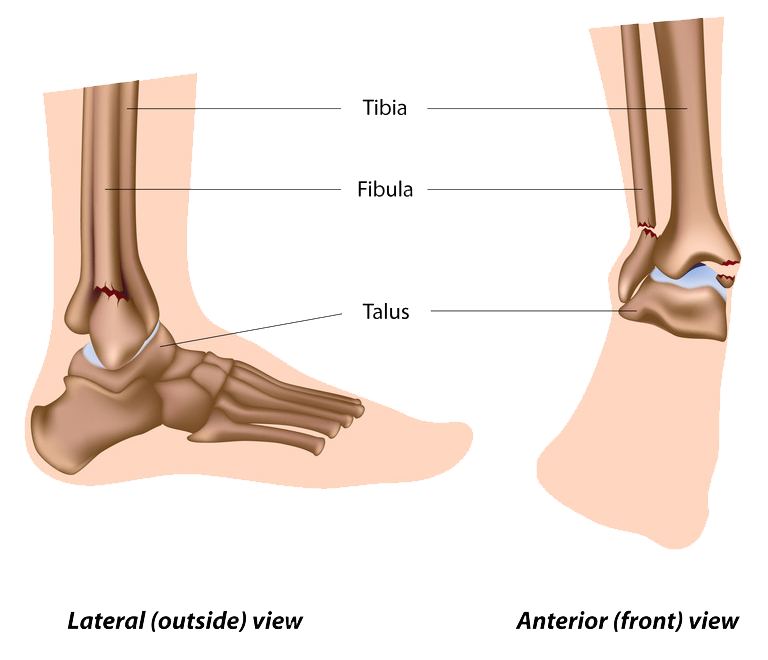
Ankle Sprains
Ankle sprains are the result of the ligaments that support the ankle stretching too much, sometimes to the point of tearing. Sprains can range from mild to severe based on how much damage is caused to the ligament. It is important to note that a severe sprain can cause long-term weakness in the ankle, leaving it susceptible to further damage including chronic ankle pain and arthritis.
Causes
Sprains are often caused by a sudden twisting of the ankle, often when walking or exercising on an uneven surface, falling, or participating in sports.
Symptoms
- Swelling
- Bruising
- Tenderness to touch
- Instability of the ankle
- In severe cases, a pop might be heard or felt
Surgical Options
Surgery is rare for ankle sprains, though in cases of persistent ankle instability it may be necessary. Surgical options may include:
- Arthroscopy, which involves the use of a very small camera and miniature instruments to remove any loose fragments of bone, cartilage, or ligament that are caught in the joint.
- Torn ligaments may need to be repaired with stiches/sutures. The doctor may need to reconstruct the ligament using a tissue graft.
Non-Surgical Options
Generally, ankle sprains can be treated without surgery, especially if the ankle is immobilized as soon as possible after the injury
Most specialists recommend a 3-phase treatment plan for sprained ankles. Phase 1 is resting and protecting the ankle to reduce the swelling. Phase 2 includes restoring range of motion, strength, and flexibility. Phase 3 is the maintenance phase, where the patient does special ankle exercises and modifies activities.
Treatment time varies from 2 weeks for minor sprains to up to 6 to 12 weeks for more severe injuries.
RICE protocol
- Rest the ankle by not walking on it.
- Ice should be immediately applied to keep the swelling down. It can be used for 20 to 30 minutes, three or four times daily. Do not apply ice directly to the skin.
- Compression dressings, bandages, or ace-wraps will immobilize and support the injured ankle.
- Elevate the ankle above the heart as often as possible during the first 48 hours.
Crutches. Due to swelling and pain, walking is often difficult and the use of crutches may be needed.
Immobilization. Support devices such as casts or braces may be necessary for a few weeks to help support and immobilize the ankle.
Physical therapy. A doctor may recommend a special program such as agility, strengthening, and balancing exercises to help treat the sprained ankle and prevent further problems.
Ruptured Ankle Ligament
In a normal ligament sprain, the lateral ankle ligament is still able to stabilize the ankle. An ankle ligament rupture means that the ligament ends are no longer in continuity, so the ligament cannot stabilize its joint. If the ligament has ruptured, the ankle may become unstable after the initial injury phase passes. Over time, this instability can result in damage to the bones and cartilage of the ankle joint.
Symptoms
- Swelling
- Bruising
- Tenderness to touch
- A popping noise at the time of injury
- Instability of the ankle— especially when there is complete dislocation of the ankle joint along with ligament rupture

Surgical Options
- Arthroscopy. During arthroscopy, a small camera called an arthroscope is used to look inside the ankle joint. Any loose fragments of bone or cartilage or parts of the ligament that may be caught in the joint are removed.
- Reconstruction. Ruptured ligaments may be repaired with stitches or sutures. In severe cases, the damaged ligament may be replaced with a tissue graft obtained from other ligaments and/or tendons found in the foot and around the ankle.
Non-Surgical Options
Initial treatment of ligament ruptures is similar to that for ankle sprains, however, due to the severity, further surgical treatment is often necessary. Nonsurgical options include:
RICE protocol
- Rest your ankle by not walking on it.
- Ice should be immediately applied to keep the swelling down. It can be used for 20 to 30 minutes, three or four times daily. Do not apply ice directly to your skin.
- Compression dressings, bandages or ace-wraps will immobilize and support your injured ankle.
- Elevate your ankle above the level of your heart as often as possible during the first 48 hours.
Crutches. Due to swelling and pain, walking is often difficult and the use of crutches may be needed.
Immobilization. Support devices such as casts or braces may be necessary for a few weeks to help support and immobilize the ankle.
Physical therapy. A doctor may recommend a special program such as agility, strengthening, and balancing exercises to help treat the sprained ankle and prevent further problems.
Plantar Fasciitis
The Plantar fascia is a long and thin ligament under the skin on the bottom of the foot that connects the heel to the front of the foot. The plantar fascia absorbs the stress and strain placed on the feet, but when too much pressure occurs it can cause tears or damage to the tissues. This results in inflammation as well as pain in the heel and stiffness.
Certain factors make some individuals more at risk of plantar fasciitis than others. These factors include:
- Tight calf muscles that make it difficult to flex the foot and bring the toes up toward the shin
- Obesity
- Very high arches
- Repetitive impact activity (running/sports)
- New or increased activity
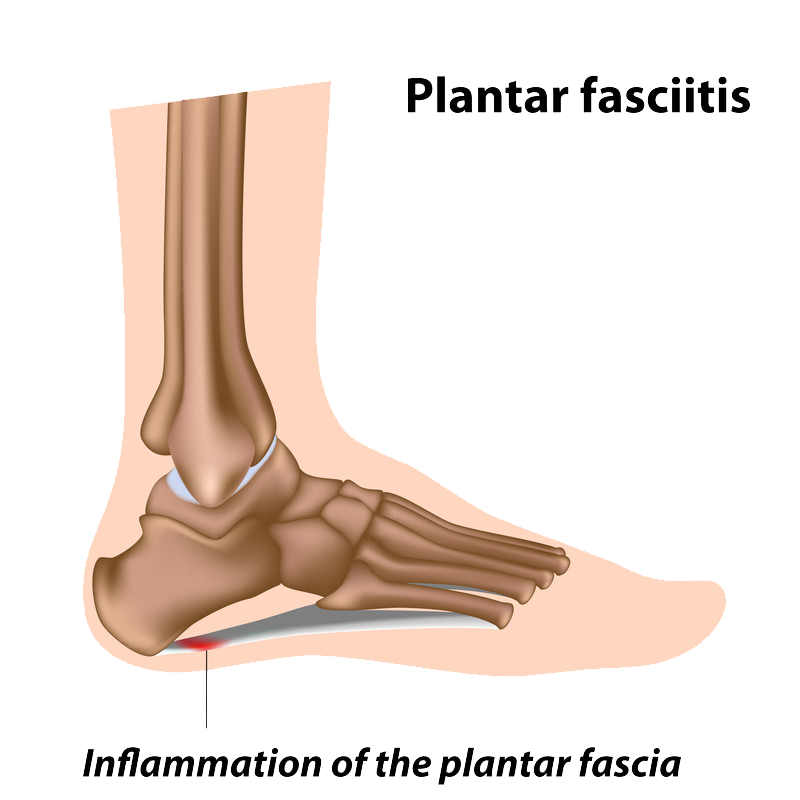
Symptoms
The most common symptoms of plantar fasciitis include:
- Pain on the bottom of the foot towards the heel
- Pain with the first few steps after getting out of bed in the morning, or after a long period of rest, such as after a long car ride. The pain subsides after a few minutes of walking
- Greater pain after (not during) exercise or activity
Surgical Options
Surgery is considered only after 12 months of aggressive nonsurgical treatment.
Gastrocnemius recession. This surgical procedure involves lengthening the calf (gastrocnemius) muscles. When calf muscles are too tight, they place increased stress on the plantar fascia. Lengthening the calf muscle assists in increasing the motion of the ankle. The procedure can be performed with a traditional open incision or with a smaller incision and an endoscope.
Plantar fascia release. If the patient has a normal range of ankle motion and continued heel pain, a doctor may recommend a partial release procedure. In this procedure, the plantar fascia ligament is partially cut to relieve tension in the tissue. This surgery can be performed endoscopically, but open surgery is less likely to cause nerve damage.
Non-Surgical Options
More than 90% of patients with plantar fasciitis will improve within 10 months of starting simple , non-surgical treatment methods.
Rest. Stopping or the activities that make the pain worse is the first step towards reducing pain. The patient may need to stop athletic activities where the feet pound on hard surfaces (for example, running or step aerobics).
Ice. Rolling the foot over a cold water bottle or ice for 20 minutes is effective. This can be done 3 to 4 times a day.
Non-steroidal anti-inflammatory medication. Ibuprofen or naproxen reduce pain and inflammation.
Exercise. Plantar fasciitis is aggravated by tight muscles in the feet and calves. Stretching the calves and plantar fascia is the most effective way to relieve the pain that comes with this condition.
Cortisone injections. Cortisone, which is a type of steroid, acts as a powerful anti-inflammatory. When injected into the plantar fascia it can reduce inflammation and pain.
Supportive shoes and orthotics. Shoes with thick soles and extra cushioning can reduce the pain of standing and walking. Pre-made or custom orthotics are also helpful.
Night splints. A splint that is used during sleeping can help stretch the plantar fascia while the patient sleeps. Although it can be difficult to sleep with a night splint, they are very effective and do not have to be used once the pain is gone.
Physical therapy. A physical therapist may recommend an exercise program that helps to stretch the calf muscles and plantar fascia.
Extracorporeal shockwave therapy (ESWT). During this procedure, high-energy shockwave impulses stimulate the healing process in damaged plantar fascia tissue. This procedure is not commonly performed, thought it has proven effective.
Bunions
A patient with a bunion will see that the joint at the base of the big toe has bulged out along the side of the foot. In that characteristic “bump,” the patient can actually seeing the effect of additional bone formation in the joint and a mechanical mis-alignment of the big toe. A bunion causes the big toe to angle toward the smaller toes. This abnormal and often painful position is referred to as hallux valgus or hallux abducto valgus.
Although bunions affect women much more often than men, tight-fitting and high-heeled shoes are not the sole cause of bunions. Ill-fitting shoes may add to the problem, but some inherited factors may predispose certain people to the formation of bunions, including congenital abnormalities in bone formation, rheumatoid arthritis, nerve conditions, and injury.
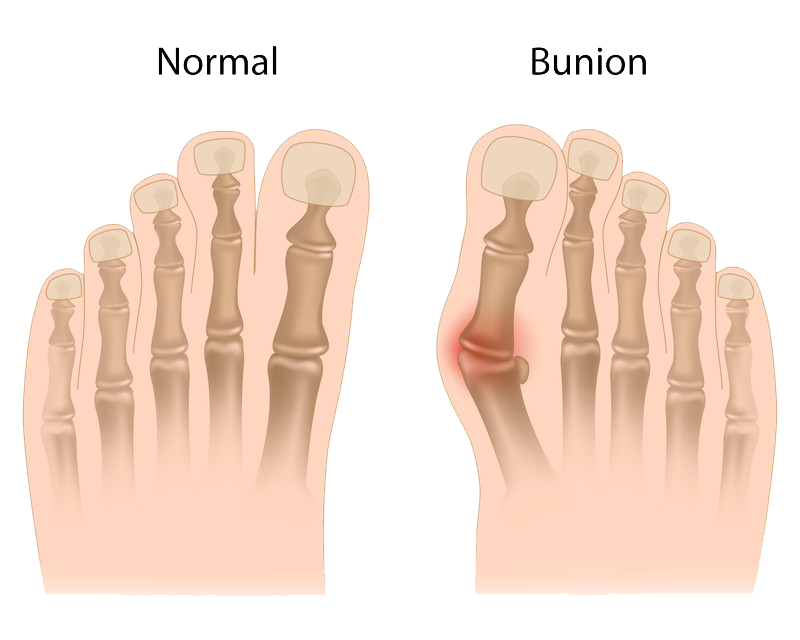
Symptoms
Sometimes bunions cause no symptoms whatsoever, but most bunions cause intermittent or chronic pain at the base of the big toe. The pain may be worse when walking or wearing shoes, and it may feel better when resting. Very painful bunions may appear red and swollen and feel tender to the touch.
Surgical Options
Bunion Surgery
Some people with bunions are able to find relief with non-surgical treatment methods to help reduce pain and pressure. When these treatments are not successful, bunion surgery may be necessary. The aim of bunion surgery is to bring the big toe back to its original position, and the surgery may involve realigning ligaments, tendons, nerves, or bones.
Non-Surgical Options
- Physical therapy
- Use of padding, orthotics, or gel inserts for footwear
- Pain relief medication
- ICE to relieve symptoms
Flat Foot
Flat foot is a condition that results in a fallen arch, forcing the foot to point outwards. There are a number of health conditions that can lead to flat foot, including:
- Anatomy of the foot and ankle. When the posterior tibial tendon is damaged, flat foot may occur. The main function of this tendon is to hold up the arch. When it is torn or inflamed, the arch may start to gradually collapse. Problems with the posterior tibial tendon are more likely to occur in those over 40, especially women and people affected by diabetes or obesity and hypertension. Participating in high impact sports can often result in tears.
- Arthritis. Arthritis that causes inflammation – such as rheumatoid arthritis – can cause flat foot. Because this type of arthritis attacks not only the cartilage in the joints but also the ligaments that support the foot, it can cause pain and change the shape of the foot.
- Injury. The ligaments in the foot may fall out of alignment when injured. Because ligaments support the bones, tears can cause the foot to become flat and painful. Fractures and dislocations may also lead to flat foot.
- Diabetic Collapse (Charcot Foot). Diabetes or nerve problems may lead to flat foot.
Symptoms
- Pain along the posterior tibial tendon. There may also be swelling on the inside of the ankle.
- Pain that becomes worse with movement. Difficulty running or participating in sports.
- Pain on the outside of the ankle caused by bones shifting position. Arthritis in the heel also causes this type of pain.
- Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps (spurs) on the top and inside of the foot. In severe cases, the bumps may pinch the nerves, resulting in numbness and tingling on the top of the foot and into the toes.
- Diabetics may notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems. An ulcer may develop if proper diabetic footwear is not used.
Surgical Options
Surgery is not performed solely to correct flat feet. However, an individual might have surgery for an associated problem such as a tendon tear or rupture.
Non-Surgical Options
Orthotics. Over-the-counter or customized arch supports may help relieve the pain caused by flat feet.
Stretching exercises. Some people with flat feet also have a shortened achilles tendon. Exercises to stretch this tendon may help.
Supportive shoes. Wearing shoes that offer good structural support can help ease symptoms.
Physical therapy. A physical therapist may offer techniques on how to walk and run in a way that offers more support and less pain.
Hammer Toe & Claw Toe
A hammer toe is a deformity of the second, third, or fourth toes. The name is given because the toe is bent at the middle joint and is said to look like a hammer. Though hammer toes are flexible initially, if left untreated they can become fixed in that position. Corns or calluses on the top of the middle joint of the toe often accompany hammer toe. Hammer toe can be caused by shoes that do not fit correctly or by a muscle imbalance in the toe.
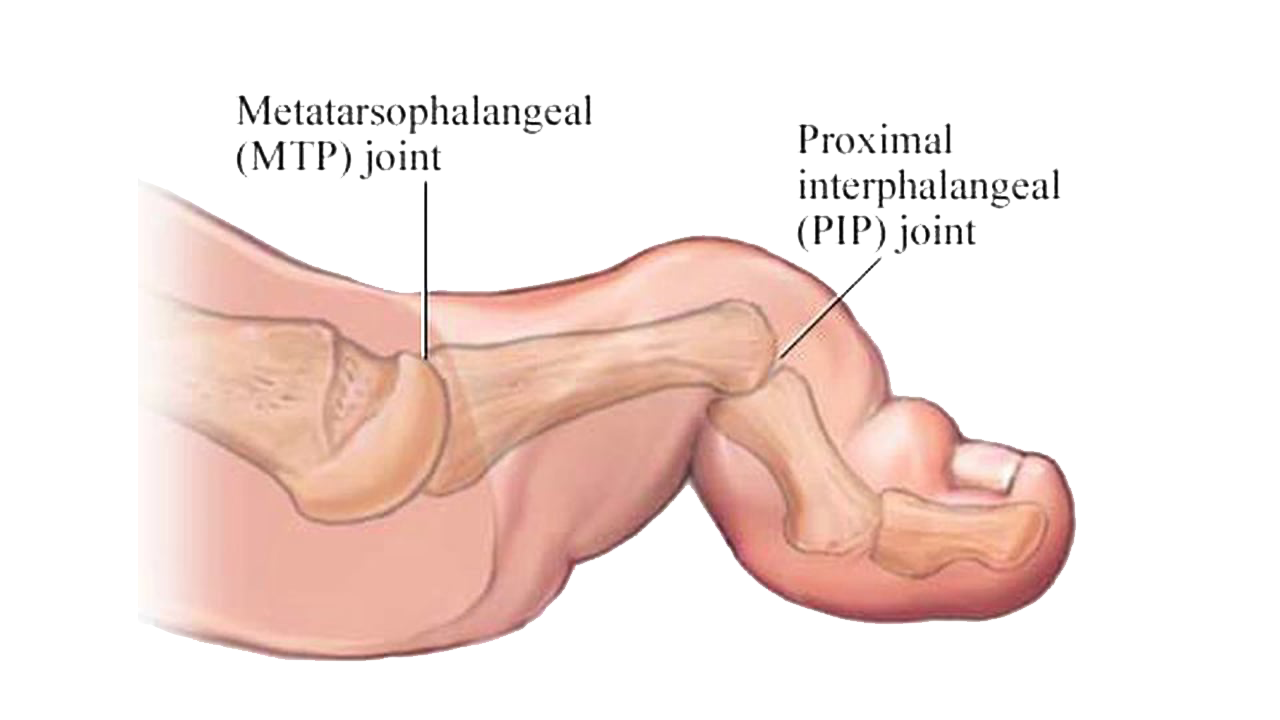
Symptoms
Symptoms of Claw Toe
- The toes are bent upward from the joints at the ball of the foot
- The toes are bent downward at the middle joints toward the sole of your shoe
- Sometimes the toes bend downward at the top joints, curling under the foot
- Corns may develop over the top of the toe or under the ball of the foot
Symptoms of Hammer Toe
- Pain at the top of the bent toe when putting on a shoe
- Corns forming on the top of the toe joint
- The toe joint swelling and taking on a red color
- Difficulty in moving the toe joint
- Pain on the ball of the foot under the bent toe
Surgical Options
Hammer toe can be corrected by surgery if conservative measures fail. Usually, surgery is done on an outpatient basis with a local anesthetic. The actual procedure will depend on the type and extent of the deformity.
Non-Surgical Options
- Footwear modification. Choosing shoes that are soft and big enough for the feet. Narrow, tight high-heeled shoes should be avoided.
- Physical therapy. A doctor may prescribe toe exercises to stretch and strengthen the muscles.
- Special equipment. Straps, cushions, or non-medicated corn pads may help relieve symptoms. If the patient has diabetes, poor circulation, or a lack of feeling in the feet, talk to a doctor before attempting any self-treatment.
Achilles Tendon Rupture
The achilles tendon may tear if it is overstretched, usually while playing sports. The tear may be partial or complete, and it most commonly occurs just above the heel bone.

Symptoms
A snap or crack sound may be heard at the time of injury. Pain and swelling near the heel and an inability to bend the foot downward or walk normally are signs that the tendon may be ruptured.
Surgical Options
Surgery is typically needed for a complete rupture. After surgery, the ankle will be kept stable in a cast or walking boot for up to 12 weeks. Surgery offers a better chance of full recovery than non-surgery, and it is often the treatment of choice for active people who wish to resume sports.
Non-Surgical Options
A torn ligament may also be managed non-surgically with a below-knee cast, which allows the ends of the torn tendon to heal on its own. This non-surgical approach may take longer to heal and there is a higher chance that the tendon could re-rupture.
Dr. Sima is our “family” doctor. He’s done wonders with my husband’s ankle (ligament replacement) and knees and my Dad’s hip.
-Denise Conte