Shoulder Injuries
Shoulder injuries are painful and inconvenient. It is important to quickly identify what your injury is and what your treatment options may be. Below you will find symptoms, treatment options, and other information about various shoulder injuries. Please contact us to request an orthopaedic evaluation.
Rotator Cuff
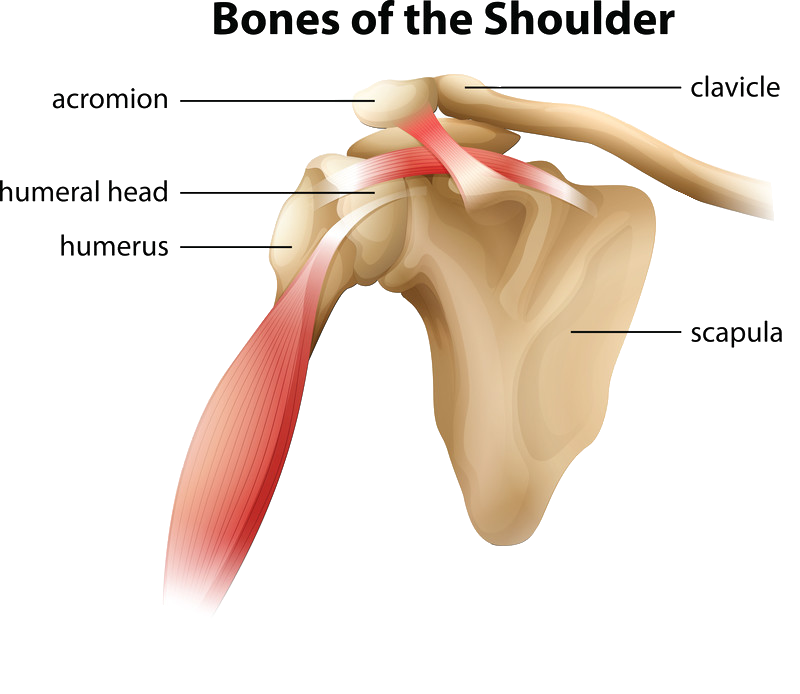
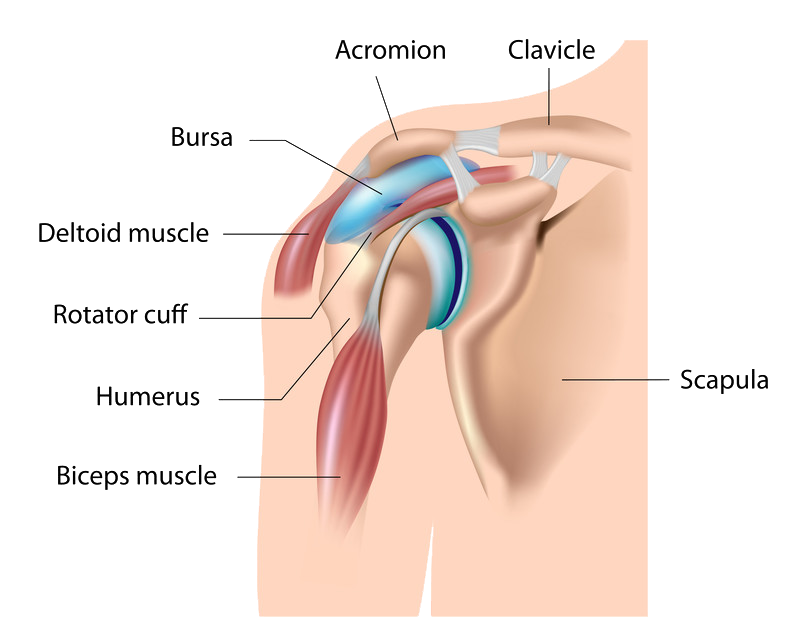
The shoulder is made up of three bones: the upper arm bone (humerus),the shoulder blade (scapula), and the collarbone (clavicle). The ball (head) of the upper arm bone fits into the socket of the shoulder blade.
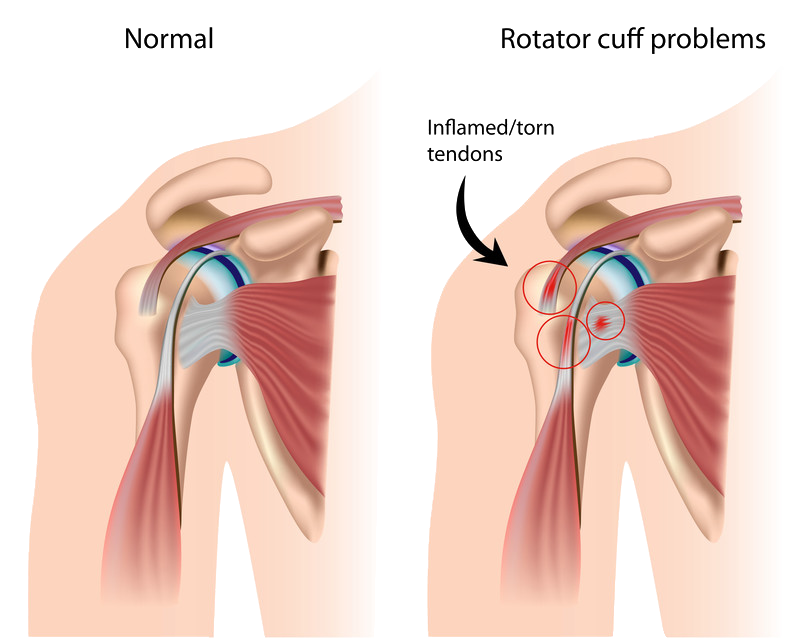
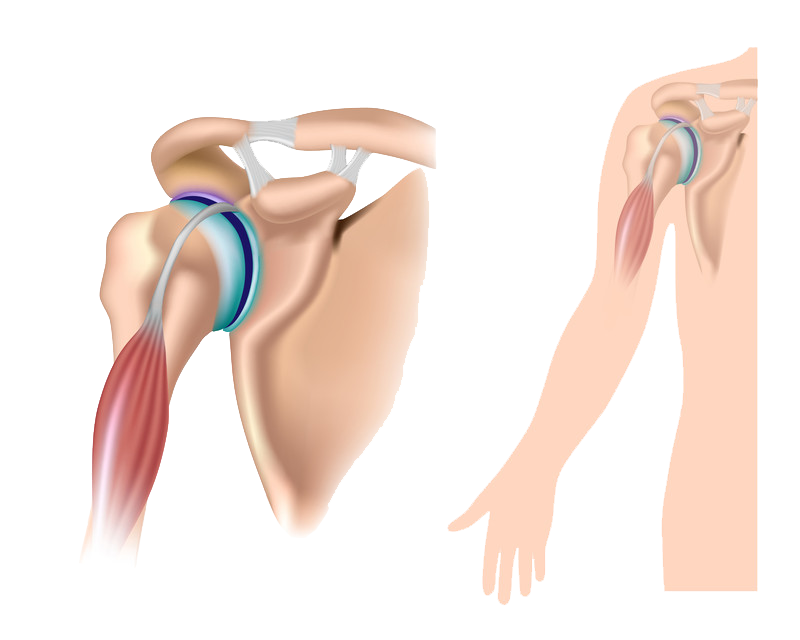
The arm is kept in the shoulder socket by the rotator cuff. The rotator cuff is a network of four muscles that come together to form a covering around the head of the humerus as tendons. The rotator cuff attaches the humerus to the shoulder blade and helps to lift and rotate the arm.
The lubricating sac called a bursa sits between the rotator cuff and the bone on top of the shoulder (acromion). In a healthy shoulder, the rotator cuff tendons glide freely when the arm is moved, but when rotator cuff tendons are injured or damaged, the bursa can become inflamed and painful.
A rotator cuff injury (tear) can cause a lot of pain and disruption to normal daily activities. When one or more of the rotator cuff tendons is torn, the tendon may no longer be attached to the head of the humerus. The most common tears occur in the supraspinatus muscle and tendon, but other parts of the rotator cuff may also be involved.
Causes of a Rotator Cuff Tear
There are two main causes of rotator cuff tears: injury and degeneration.
Acute Tear. If you fall down on your outstretched arm or lift something too heavy with a jerking motion, you can tear your rotator cuff. This type of tear can occur with other shoulder injuries, such as a broken collarbone or dislocated shoulder.
Degenerative Tear. Most tears are the result of a wearing down of the tendon that occurs slowly over time. This degeneration naturally occurs as we age. Rotator cuff tears are more common in the dominant arm. If you have a degenerative tear in one shoulder, there is a greater risk for a rotator cuff tear in the opposite shoulder — even if you have no pain in that shoulder.
Several factors contribute to degenerative, or chronic, rotator cuff tears.
- Repetitive stress. Repeating the same shoulder motions again and again can stress your rotator cuff muscles and tendons. Baseball, tennis, rowing, and weightlifting are examples of sports activities that can put you at risk for overuse tears. Many jobs and routine chores can cause overuse tears, as well.
- Lack of blood supply. As we get older, the blood supply in our rotator cuff tendons lessens. Without a good blood supply, the body’s natural ability to repair tendon damage is impaired. This can ultimately lead to a tendon tear.
- Bone spurs. As we age, bone spurs (bone overgrowth) often develop on the underside of the acromion bone. When we lift our arms, the spurs rub on the rotator cuff tendon. This condition is called shoulder impingement, and over time will weaken the tendon and make it more likely to tear.
Risk Factors
Because most rotator cuff tears are largely caused by the normal wear and tear that goes along with aging, people over 40 are at greater risk.
People who do repetitive lifting or overhead activities are also at risk for rotator cuff tears. Athletes are especially vulnerable to overuse tears, particularly tennis players and baseball pitchers. Painters, carpenters, and others who do overhead work also have a greater chance for tears.
Although overuse tears caused by sports activity or overhead work also occur in younger people, most tears in young adults are caused by a traumatic injury, like a fall.
Symptoms
The symptoms of a rotator cuff tear depend on the cause. Tears caused by trauma may create an immediate and sharp pain in the shoulder and weakness in the arm. Tears caused by overuse may create pain that begins as a minor twinge when lifting the arm. With overuse injuries, pain may develop into chronic distress in the shoulder that radiates and limits arm and shoulder movements. Pain may even interrupt sleep.
Surgical Options
Surgery may be necessary if non-surgical methods haven’t helped, or if the chance of further damage is high.
Surgery is also recommended if:
- The damage was recently caused by a severe injury
- The symptoms have lasted more than 6 months
- The tear is larger than 3cm
- The weakness or loss of mobility in the shoulder is severe
Surgery to repair a torn rotator cuff most often involves re-attaching the tendon to the head of humerus (upper arm bone). There are a few options for repairing rotator cuff tears, and Dr. Sima is happy to discuss the particulars of the procedure with interested patients.
Non-Surgical Options
While shoulder strength generally does not improve without surgery, non-surgical treatment may assist with easing pain and increasing mobility. Check out the latest medical advancements in surgery alternatives for shoulder injuries.
- Resting the shoulder
Limiting activities, and providing additional support such as a sling
- Modifying / Changing activities
Cutting back on actions that cause pain or discomfort, or modifying the way actions are performed
- Non-steroidal anti-inflammatory medication (NSAIDS)
Medication helps reduce pain and swelling (for example ibuprofen and naproxen)
- Physical therapy
The doctor may recommend a customized exercise program to help improve flexibility and motion. Stretching may help restore movement and strengthen the muscles, causing some pain relief.
- Steroid injection
Cortisone can be a very effective anti-inflammatory medicine, but is generally reserved for use if other interventions haven’t helped.
Shoulder Arthritis
Arthritis is a common and sometimes debilitating condition caused by inflammation of the joints. In the shoulder, arthritis causes pain, stiffness, and reduced mobility, sometimes having a major effect on general day-to-day activities. Arthritis has no cure, though Dr. Sima can explain treatment options that will help with pain management and will allow patients to maintain an active lifestyle.
Types of Arthritis
Osteoarthritis (Degenerative Joint Disease)
Osteoarthritis is typically related to stress and movement over time. While it is generally occurs in those over 50, it may occur in younger individuals. Because cartilage gradually wears away with use over time, the bones start to move against each other without sufficient protection. This is what causes shoulder stiffness and pain.
Rheumatoid Arthritis
Rheumatoid arthritis is a form of inflammatory arthritis that occurs when there is inflammation in the synovial membrane, causing it to become thicker. Over time, the inflammation causes damage to the cartilage, with stiffness and pain the result.
Post-Traumatic Arthritis
Arthritis that develops after a serious injury is known as post-traumatic arthritis. Torn ligaments or bone fragments from a high-impact injury can damage the articular cartilage. As time goes on, the increasing damage causes serious pain and can limit daily activities.
Avascular Necrosis (Osteonecrosis)
When blood supply is restricted to the bone, it’s known as avascular necrosis, a very painful condition. Without blood supply, the bone cells eventually die and the destruction of the shoulder joint can cause arthritis. Some risk factors include heavy alcohol use, deep sea diving, long term steroid usage, shoulder fracture, or sickle cell disease.
Symptoms
- Pain. Pain in the shoulder that gets worse with activity or comes on gradually may be a sign of arthritis. The pain may change with changes in the weather or time of day. Pain may be centered in the back or top of the shoulder, depending on which joint is affected.
- Less range of motion. The patient may experience a greater difficulty lifting the arm to complete everyday activities.
- Noise when moving the shoulder. Some patients report clicking and snapping sounds when moving the shoulder.
Surgical Options
A doctor may consider surgery if the patient’s shoulder pain causes disability and is not relieved with nonsurgical options.
Arthroscopy. Cases of mild arthritis may be treated with arthroscopy. During arthroscopy, a small camera known as an arthroscope is inserted into the shoulder. The images it transmits help the surgeon guide the surgical instruments during the shoulder procedure.
The procedure itself involves cleaning out the inside of the joint. Pain should be significantly reduced, however it cannot cure the arthritis, so further surgery may be necessary in the future.
Shoulder joint replacement is recommended when arthritis is advanced. Advanced arthritis of the glenohumeral joint can be treated with shoulder replacement surgery, in which the damaged parts of the shoulder are removed and replaced with an artificial plastic and metal parts, called a prosthesis.
Replacement surgery options include:
- Hemiarthroplasty
Only the head of the humerus is replaced with a prosthesis
The head of the humerus is replaced with a metal ball and the glenoid has a plastic cup fitted.
In reverse total shoulder replacement, the socket and metal ball are attached differently. The metal ball is attached to the shoulder bone, and a plastic socket is attached to the upper arm bone.
- Resection arthroplasty
This is an arthroscopic procedure used to treat arthritis of the acromioclavicular joint. Bone is removed from the end of the collarbone and the space created will gradually fill with scar tissue.
Non-Surgical Options
Some symptoms of arthritis can be eased with nonsurgical treatment. A specialist may suggest some of these options:
- Resting the shoulder and modifying activities to avoid pain.
- Physical therapy exercises
- Reduce pain and inflammation with nonsteroidal anti-inflammatory medications
- Corticosteroid injections may temporarily ease pain and inflammation
- Applying an ice pack to the shoulder 2 or 3 times a day. Inflammation may be reduced and pain eased if the ice is applied for 20 – 30mins each time.
- Medications (including natural supplements) may provide temporary relief but should be taken only under consultation with a qualified specialist.
Shoulder Tendonitis
Shoulder tendonitis is a common causes of stiffness and pain in the shoulder. The shoulder joint is supported by the rotator cuff and the bicipital tendon. When these tendons become inflamed it is known as tendonitis.
Symptoms
- Pain and swelling in the front of the shoulder and side of the arm.
- Pain when raising, lowering, or reaching with the arm
- Clicking noise when the arm is raised
- Stiffness in the shoulder
- Pain severe enough to interrupt sleep
Non-Surgical Options
The RICE protocol
- Rest – take a break from the activity that caused the strain, and consider using crutches to avoid putting weight on your leg
- Ice – use cold packs several times a day for up to 20 minutes at a time, remembering not to apply ice directly to the skin
- Compression – wear an elastic compression bandage to prevent additional swelling and blood loss
- Elevation – This can be tricky when it comes to the shoulder but will likely occur without added effort.
Torn Labrum
The labrum is a piece of cartilage that is joined to the shoulder socket and helps keep the ball and joint in the correct position. When the cartilage tears (through injury or long term use) it is known as a labrum (or labral) tear.
A SLAP lesion (which stands for a tear in the Superior Labrum, Anterior to Posterior) is where the labrum is torn from the front to the back. Sudden pulls on the muscle can pull the superior labrum off the bone.
Injuries that may cause a labrum tear include:
- Falling and using an outstretched arm to stop the fall
- Sudden pulling
- Sudden reaching
- Direct impact to the shoulder
Glenoid labrum tears are common in athletes such as weightlifters or those in throwing sports because of the repetitive shoulder motion.
Symptoms
- Weakness in the shoulder
- Pain with normal daily activities, especially reaching above the head
- Instability in the shoulder
- Less range of motion
- Feeling of popping, grinding, locking, or catching
Surgical Options
Through arthroscopic surgery, the doctor will examine the area to see if only the rim is affected. The shoulder will be stable if the tendon hasn’t torn. The doctor will then perform labral repair.
- The torn fragment will be removed and other minor damage treated
- If the tendon has detached, or the tear is large, the surgeon will need to consider more detailed surgery including reattaching the tendon using wires and stitches.
- If the tear is below the middle of the socket, instability will be evident. A surgeon will need to reattach the ligament and tighten the shoulder socket.
Non-Surgical Options
- Anti-inflammatory medication
- Rest
- Change of activities to limit painful movement
- Gentle exercises
Shoulder Fracture
Fractures are broken bones. In the shoulder, fractures generally involve the scapula, clavicle (collar bone), and proximal humerus (the top of the upper arm bone). These can be caused by an accident, fall, or direct blow to the shoulder.
Dislocations occur when bones on opposite sides of a joint do not line up correctly. In the shoulder this can involve:
- The acromioclavicular joint (collar bone joint) – dislocation here is called a separated shoulder.
- The sternoclavicular joint interrupts the connection between the clavicle and the sternum
- The glenohumeral joint (the ball and socket joint of the shoulder)
Anterior dislocations are caused by the arm being forceful outward rotation. Posterior dislocations generally occur from electric shocks or seizures when the muscles are forced to contract rapidly.
Shoulder Separations are caused by a fall onto the shoulder or from heavy lifting. The acromioclavicular joint becomes dislocated.
Symptoms
Symptoms of fractures
- Pain
- Difficulty moving the shoulder
- Swelling and bruising
- A grinding feeling when moving the shoulder
- Deformity
Specific fractures have different symptoms
Fractured Clavicle (Collarbone)
- Swelling in the collarbone area
- Feeling of a lump under the skin
- Limited range of motion
Proximal Humerus Fracture
- Very severe pain
- Heavy swelling
- Limited movement of the shoulder
Scapular Fracture
- Pain
- Swelling
- Severe bruising in the shoulder blade area
Shoulder Separation (Acromioclavicular Joint Separation)
- Pain, especially at the top of the shoulder
- Feeling of a bump or something sticking up under the skin at the top of the shoulder
Shoulder Dislocation (Glenohumeral Joint Dislocation)
- Unstable shoulder
- Loss of feeling in the arm
- Unable to move the arm
- Shoulder sticking out at the front or rotated forward
Surgical Options
Clavicle Fractures
When a compound fracture is severely out of place, or the bone has broken through the skin surgery becomes necessary. Surgery will generally involve fixing the fracture with metal screws and plates inside the bone.
Proximal Humerus Fractures
When a proximal humerus fracture has caused fragments to shift out of position, surgery is required. This procedure involves using plates, pins, and screws to repair the fracture. If severe enough, shoulder replacement surgery may be required
Scapula Fractures
Surgical treatment of a scapula fracture is necessary when the fracture fragments involve the shoulder joint or if there is an additional fracture (especially to the clavicle). The fracture is repaired with metal plates and screws.
Shoulder Separations (Acromioclavicular Joint)
Severe separations that occur in an upward direction or dislocations in the backward or downward directions often require surgery. This surgery aims to repair the ligaments damaged by the separation in the acromioclavicular joint.
Shoulder Dislocations (Glenohumeral Joint)
The first step in treating shoulder dislocation is generally manipulating the shoulder components until the dislocated area slots back into the correct position. This procedure is obviously quite painful and should take place in an emergency room under sedation. Further surgery involving the repair of soft tissue tears may be necessary.
Non-Surgical Options
Some fractures can be treated without surgery. Treatment may include:
- PRP may be a solution for some fractures.
- Slings, collars, and other devices to immobilize the area
- Limiting use of the affected shoulder
- Gentle exercises to strengthen the area
- Direct manipulation (gently moving the bones to help place them correctly)
Shoulder Bursitis
Bursae are sacs containing fluid that are found in all joints. They help protect bones and soft tissue by providing cushioning, reducing the friction caused by moving muscle and bones.
If the shoulder is used too repetitively it may lead to inflammation of the bursa, between the rotator cuff and the acromion region of the shoulder blade. This condition is known as subacromonial bursitis. Bursitis may also occur in conjunction with rotator cuff tendinitis.
Causes of Bursitis:
- Trauma/injury
- Long term use
- Infection
- Underlying conditions (such as arthritis)
Symptoms of Bursitis
- Symptoms usually show up gradually over weeks or months
- Painful movements
Surgical Options
Infected bursae that do not respond to antibiotics or fluid drainage, or bursitis not caused by infection but not improving with other methods, may be removed entirely through an inpatient procedure. Healthy bursae will then grow back over a period of months.
Non-Surgical Options
- Aspiration (removing the fluid) from the bursa with a needle if an infection is suspected, antibiotics are generally given in addition to the procedure
- Activity modification – avoiding actions that cause pain to the shoulder
- Applying a sling to help support the shoulder and restrict painful activities
- Applying an ice pack may provide temporary relief to pain and swelling
- Anti-inflammatory and pain killing medications may help ease inflammation and pain. Corticosteroid medication may be injected if pain and inflammation isn’t relieved through other methods.
Biceps Tendon Tear at the Shoulder
Tendons attach muscles to bones. Your biceps tendons attach the biceps muscle to bones in the shoulder and in the elbow. If you tear the biceps tendon at the shoulder, you may lose some strength in your arm and have pain when you forcefully turn your arm from palm down to palm up.
Many people can still function with a biceps tendon tear, and only need simple treatments to relieve symptoms. If symptoms cannot be relieved by nonsurgical treatments, or if a patient requires complete recovery of strength, surgery to repair the torn tendon may be required.
Causes:
There are two main causes of biceps tendon tears: injury and overuse.
- Injury. If you fall hard on an outstretched arm or lift something too heavy, you can tear your biceps tendon.
- Overuse. Many tears are the result of a wearing down and fraying of the tendon that occurs slowly over time. This naturally occurs as we age. It can be worsened by overuse – repeating the same shoulder motions again and again.Overuse can cause a range of shoulder problems, including tendinitis, shoulder impingement, and rotator cuff injuries. Having any of these conditions puts more stress on the biceps tendon, making it more likely to weaken or tear.
Risk Factors
Your risk for a tendon tear increases with:
- Age. Older people have put more years of wear and tear on their tendons than younger people.
- Heavy overhead activities. Too much load during weightlifting is a prime example of this risk, but many jobs require heavy overhead lifting and put excess wear and tear on the tendons.
- Shoulder overuse. Repetitive overhead sports, such as swimming or tennis, can cause more tendon wear and tear.
- Smoking. Nicotine use can affect nutrition in the tendon.
- Corticosteroid medications. Using corticosteroids has been linked to increased muscle and tendon weakness.
Surgical Options
Surgical treatment for a long head of the biceps tendon tear is rarely needed. However, some patients who develop cramping of the muscle or pain, or who require complete recovery of strength, such as athletes or manual laborers, may require surgery. Surgery may also be the right option for those with partial tears whose symptoms are not relieved with nonsurgical treatment.
Procedure. Several new procedures have been developed that repair the tendon with minimal incisions. The goal of the surgery is to re-anchor the torn tendon back to the bone. Your doctor will discuss with you the options that are best for your specific case.
Complications. Complications with this surgery are rare. Re-rupture of the repaired tendon is uncommon.
Rehabilitation. After surgery, your shoulder may be immobilized temporarily with a sling.
Your doctor will soon start you on therapeutic exercises. Flexibility exercises will improve range of motion in your shoulder. Exercises to strengthen your shoulder will gradually be added to your rehabilitation plan.
Be sure to follow your doctor’s treatment plan. Although it is a slow process, your commitment to physical therapy is the most important factor in returning to all the activities you enjoy.
Surgical Outcome. Successful surgery can correct muscle deformity and return your arm’s strength and function to nearly normal.
Non-Surgical Options
For many people, pain from a long head of biceps tendon tear resolves over time. Mild arm weakness or arm deformity may not bother some patients, such as older and less active people.
In addition, if you have not damaged a more critical structure, such as the rotator cuff, nonsurgical treatment is a reasonable option. This can include:
- Ice. Apply cold packs for 20 minutes at a time, several times a day to keep down swelling. Do not apply ice directly to the skin.
- Nonsteroidal anti-inflammatory medications. Drugs like ibuprofen, aspirin, or naproxen reduce pain and swelling.
- Rest. Avoid heavy lifting and overhead activities to relieve pain and limit swelling. Your doctor may recommend using a sling for a brief time.
- Physical therapy. Flexibility and strengthening exercises will restore movement and strengthen your shoulder.
Impingement Syndrome
One of the most common physical complaints is shoulder pain. Your shoulder is made up of several joints combined with tendons and muscles that allow a great range of motion in your arm. Because so many different structures make up the shoulder, it is vulnerable to many different problems. The rotator cuff is a frequent source of pain in the shoulder.
Description
The rotator cuff is a common source of pain in the shoulder. Pain can be the result of:
- Tendinitis. The rotator cuff tendons can be irritated or damaged.
- Bursitis. The bursa can become inflamed and swell with more fluid causing pain.
- Impingement. When you raise your arm to shoulder height, the space between the acromion and rotator cuff narrows. The acromion can rub against (or “impinge” on) the tendon and the bursa, causing irritation and pain.
Symptoms of Impingement Syndrome
Rotator cuff pain commonly causes local swelling and tenderness in the front of the shoulder. You may have pain and stiffness when you lift your arm. There may also be pain when the arm is lowered from an elevated position.
Beginning symptoms may be mild. Patients frequently do not seek treatment at an early stage. These symptoms may include:
- Minor pain that is present both with activity and at rest
- Pain radiating from the front of the shoulder to the side of the arm
- Sudden pain with lifting and reaching movements
- Athletes in overhead sports may have pain when throwing or serving a tennis ball
As the problem progresses, the symptoms increase:
- Pain at night
- Loss of strength and motion
- Difficulty doing activities that place the arm behind the back, such as buttoning or zippering
If the pain comes on suddenly, the shoulder may be severely tender. All movement may be limited and painful.
Surgical Options
Arthroscopic technique. In arthroscopy, thin surgical instruments are inserted into two or three small puncture wounds around your shoulder. Your doctor examines your shoulder through a fiberoptic scope connected to a television camera. He or she guides the small instruments using a video monitor, and removes bone and soft tissue. In most cases, the front edge of the acromion is removed along with some of the bursal tissue.
Your surgeon may also treat other conditions present in the shoulder at the time of surgery. These can include arthritis between the clavicle (collarbone) and the acromion (acromioclavicular arthritis), inflammation of the biceps tendon (biceps tendonitis), or a partial rotator cuff tear.
Non-Surgical Options
In most cases, initial treatment is nonsurgical. Although nonsurgical treatment may take several weeks to months, many patients experience a gradual improvement and return to function.
Rest. Your doctor may suggest rest and activity modification, such as avoiding overhead activities.
Non-steroidal anti-inflammatory medicines. Drugs like ibuprofen and naproxen reduce pain and swelling.
Physical therapy. A physical therapist will initially focus on restoring normal motion to your shoulder. Stretching exercises to improve range of motion are very helpful. If you have difficulty reaching behind your back, you may have developed tightness of the posterior capsule of the shoulder (capsule refers to the inner lining of the shoulder and posterior refers to the back of the shoulder). Specific stretching of the posterior capsule can be very effective in relieving pain in the shoulder.
Once your pain is improving, your therapist can start you on a strengthening program for the rotator cuff muscles.
Steroid injection. If rest, medications, and physical therapy do not relieve your pain, an injection of a local anesthetic and a cortisone preparation may be helpful. Cortisone is a very effective anti-inflammatory medicine. Injecting it into the bursa beneath the acromion can relieve pain.
I have had three surgeries performed by Dr. Sima over this past year. The “results” of all three of the surgeries were far in excess of my expectations. Often times many people experience “excellence” within the Medical world, but rarely does a surgeon come along that is in that elite category that is above “excellent”. Dr. Sima is in that category.
-Peter Clyde